CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 4, July/August 2011
AFRICA
207
show any thrombus in the main pulmonary artery or its branches,
we decided to initiate thrombolytic therapy because of the high
risk of the massive embolus. We administered a prolonged low-
dose of recombinant tissue plasminogen activator (tPA) because
of her advanced age.
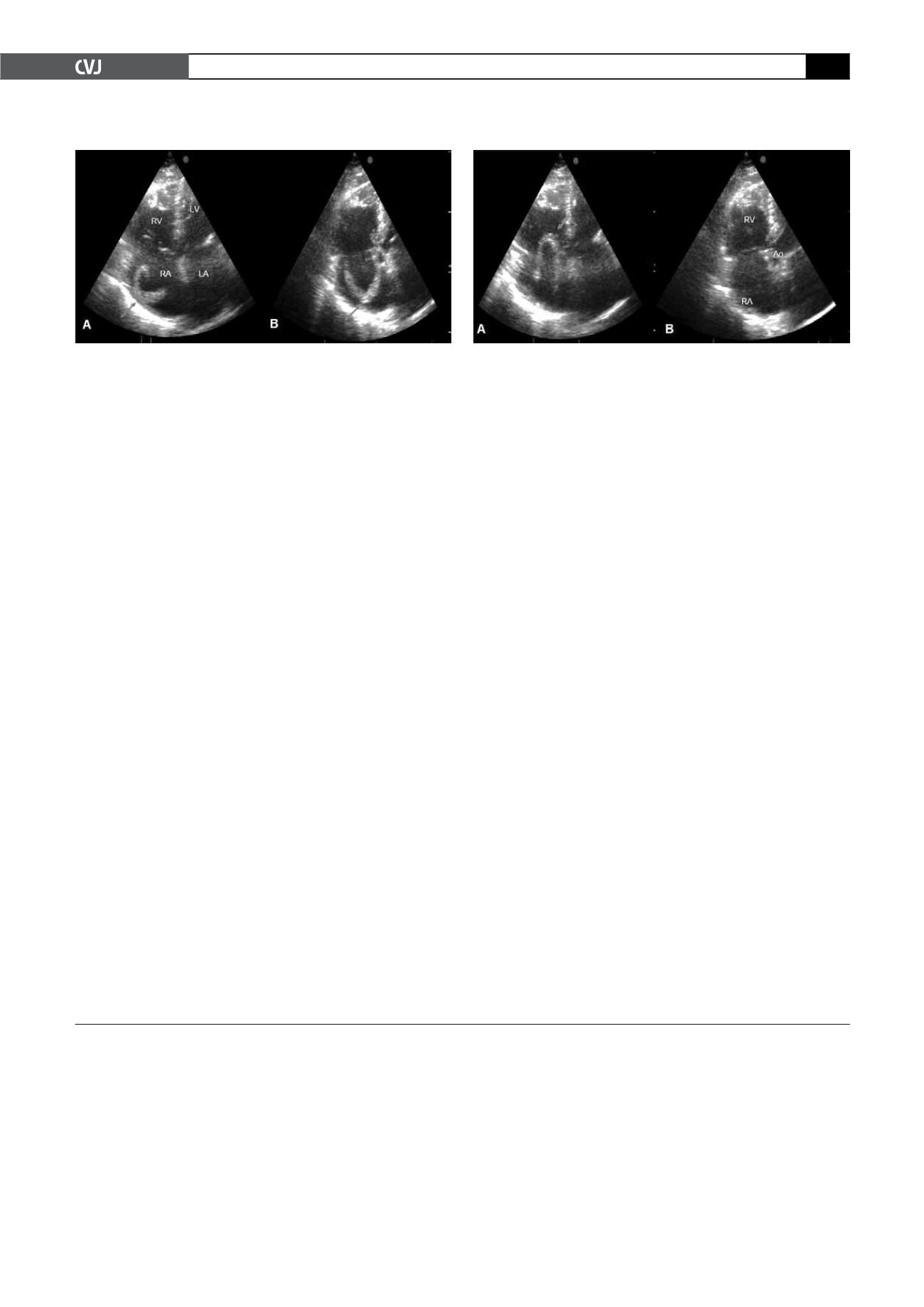
After six hours of 50-mg tPA infusion, control echocardi-
ography showed the thrombus was completely resolved, with
clinical and haemodynamic improvement (Fig. 2). There after we
administered a heparin infusion, followed by warfarin therapy.
On the third day, she was discharged on warfarin treatment with
sufficient INR levels.
Discussion
In this report, we present an elderly patient with mobile, snake-
like right atrial thrombus leading to pulmonary embolism.
Snake-like thrombus is extremely mobile and patients with this
shaped thrombus have a very poor prognosis, with a 45% mortal-
ity rate.
5
There is no generally accepted therapeutic choice. Although
embolectomy is a frequently proposed treatment, Pierre-Justin
et al
.
6
showed in a prospective study that thrombolytic therapy
with tPA appeared to be rapidly effective in most patients, result-
ing in complete resolution of the thrombus. Thrombolysis is
also advantageous for intra-cavity thrombus, for the pulmonary
pole and for deep-vein thrombosis. There is no consensus on
the thrombolytic dose or the protocol of the therapy, but the
most common dose administered is 100 mg tPA over a two-hour
infusion.
5,7
Pierre-Justin
et al
.
6
administered lower-dose tPA with
more prolonged infusions.
In this case, we used low-dose tPA in a prolonged infusion
because of the patient’s advanced age. With echocardiographic
visualisation of the right atrial thrombus, we could monitor it and
stop the thrombolytic therapy when the thrombus had resolved.
With this strategy we could avoid complications caused by the
thrombolytics.
References
1.
Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clin-
ical outcomes in the International Cooperative Pulmonary Embolism
Registry (ICOPER).
Lancet
1999;
353
: 1386–1389.
2.
Lasing E, Weber T, Auer J,
et al
. Uncommon electrocardiogram in
a patient with right atrial thrombus and pulmonary embolism.
Int J
Cardiol
2005;
103
: 345–347.
3.
Colletta M, Paoloni P, Ciliberti D,
et al
. Right atrial thrombosis and
pulmonary embolism: role of echocardiography.
Minerva Cardioangiol
1997;
45
: 439–442.
4.
Janssens U, Klues HG, Hanrath P. Successful thrombolysis of right
atrial and ventricle thrombi in a patient with peripartum cardiomyopa-
thy and extensive thromboembolism.
Heart
1997;
78
: 515–516.
5.
Peláez JB, de Miguel EM, Moreno RS,
et al
. Right-atrial floating throm-
bus attached to the interatrial septum with massive pulmonary embo-
lism diagnosed by echocardiography.
Int J Cardiol
2008;
131
: 125–127.
6.
Pierre-Justin G, Pierard LA. Management of mobile right heart throm-
bi: A prospective series.
Int J Cardiol
2005;
99
: 381–388.
7.
Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboem-
boli.
Chest
2002;
121
: 806–814.
Fig. 2. Resolution of the free-floating thrombus. RA: right
atrium, RV: right ventricle, Ao: aorta.
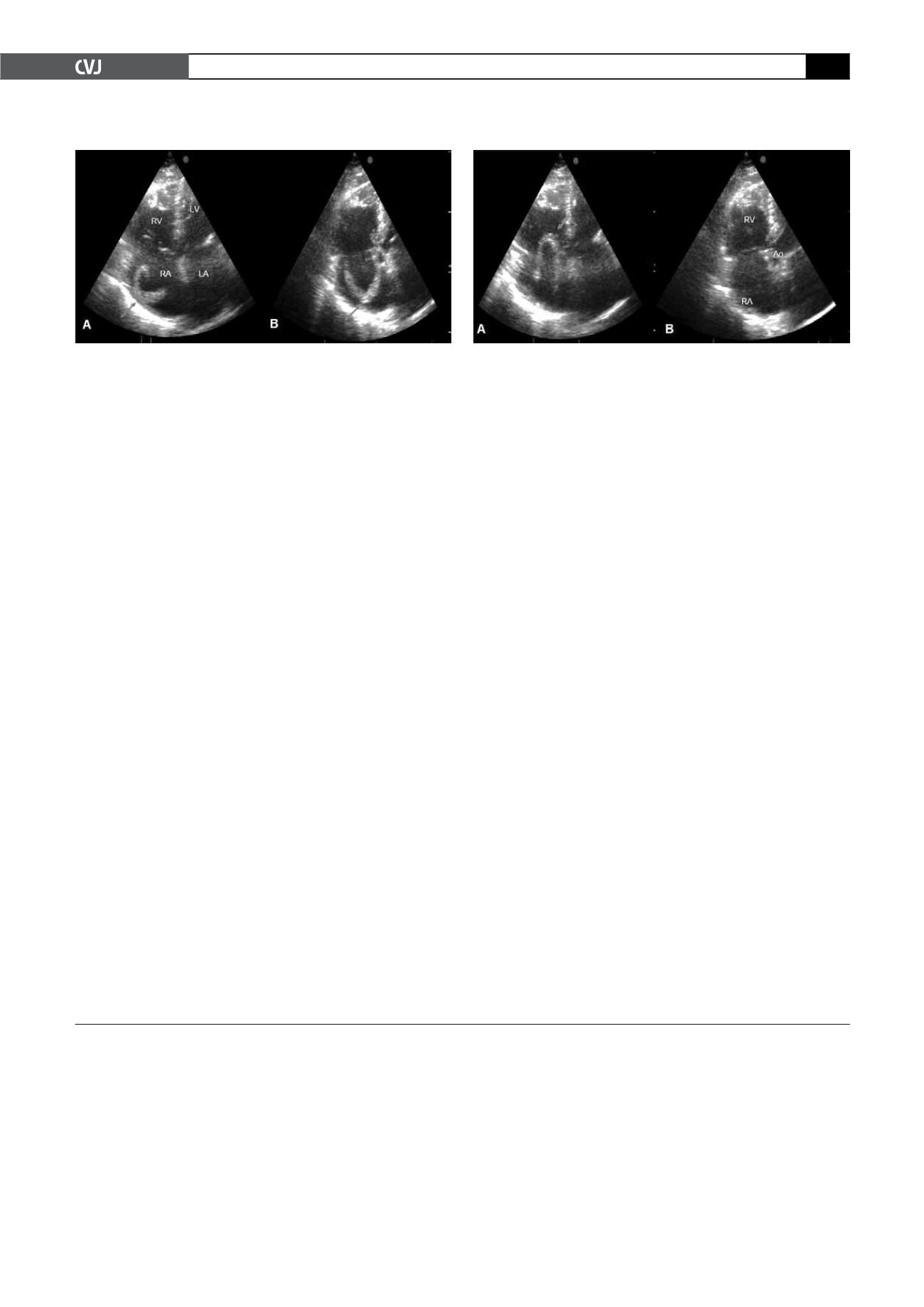
Fig. 1. Apical four-chamber views of a snake-like throm-
bus floating in the right atrium. RA: right atrium, RV: right
ventricle, LA: left atrium, LV: left ventricle. The thrombus
is indicated with an arrow.