CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 10, November 2012
544
AFRICA
The association of LQT with an elevated LVEDP (at a normal
LVEF – frequently defined as
>
45% ,
and used for the purpose
of this study) is striking. Diastolic dysfunction is a relatively new
concept when compared with LVEF. The commonest cause of
diastolic dysfunction is hypertensive heart disease. Often these
patients have thicker, stiffened left ventricles with good systolic
function, but impaired relaxation and compliance. Again, exactly
how diastolic dysfunction in IHD patients is associated with
QT prolongation remains unknown, but recently an association
was found between down-regulation of the hERG gene and QT
prolongation in rats with cardiac hypertrophy.
34
Ion-channels are embedded in a phospholipid bi-layer
primarily composed of cholesterol esters. Both congenital
LQTS and familial hypercholesterolaemia are more common
in South Africans of European descent. Co-segregation of
ion-channel disease and hypercholesterolaemia has not yet
been described in humans, but in Langendorff-perfused rabbit
hearts, hyperlipidaemia led to significant QT prolongation
compared with normocholesterolaemia, which can be reversed
by administering simvastatin.
35
Study limitations
This single-centre study in a state hospital setting may be prone
to selection bias due to the fact that patients were enrolled only
during rotations of the authors collecting the data through the
coronary care unit. However, all eligible patients were enrolled
during these intervals, leading us to believe that the cohort was
truly representative.
More than 80% of the studied population were of mixed racial
ancestry. One should therefore be careful to draw conclusions
about race and QT prolongation.
Prescribed medications were not checked and these may well
have prolonged the QT interval after discharge. However, this
study addressed the relationship between QTc prior to coronary
angiography and mortality at six months.
The effects of coronary revascularisation on QTc were also not
investigated but it was assumed that significant coronary stenosis
would have been treated appropriately by the interventional
cardiologist. Mortality in the LQT cohort remained high
regardless of coronary revascularisation. Follow up was relatively
short owing to the vast extent of the geographical catchment area
of the hospital.
Genetic screening was also not performed on the study
patients. Diastolic pressure was used as an indicator of diastolic
function; however, echocardiographic parameters of diastolic
function were not assessed.
Conclusion
This is the first description of LQTc in a cohort of IHD patients
in a South African setting. The study confirms that QTc, which
can be determined by a simple, non-invasive, inexpensive
method, is an index of subsequent sudden death in patients who
undergo coronary angiography for suspected IHD.
QTc prolongation before coronary angiography is also a
reflection of systolic and diastolic dysfunction (in the context
of normal systolic function) of the left ventricle, both of which
are independent predictors of mortality rate. Furthermore, LQTc
correlates with hypercholesterolaemia and a negative family
history of IHD.
We are grateful to Khetha Majola and Innocentia Louw for helping with data
capturing, Prof Daan Nel of the Centre for Statistical Consultation (CSC),
Stellenbosch University, for the statistical analysis, and the Harry Crossley
Foundation for generous financial assistance. Elizabeth Schaafsma and Pearl
Fredericks were of assistance in data collection and establishment of an
electronic database.
References
1.
Reardon M, Malik M. QT interval change with age in an overtly healthy
older population.
Clin Cardiol
1996;
19
: 949–952.
2.
Beyerbach DM, Kovacs RJ, Dmitrienko AA. Heart rate-corrected QT
interval in men increases during winter months.
Heart Rhythm
2007;
4
: 277–281.
3.
Molnar J, Zhang F, Weiss J,
et al
.
Diurnal pattern of QTc interval: how
long is prolonged? Possible relation to circadian triggers of cardiovas-
cular events.
J Am Coll Cardiol
1996;
27
: 76–83.
4.
Kautzner J. QT interval measurements.
Cardiac Electrophysiol Rev
2002;
6
: 273–277.
5.
Goldenberg I, Moss AJ, Zareba W. QT interval: how to measure it and
what is “normal”.
J Cardiovasc Electrophysiol
2006;
17
: 333–336.
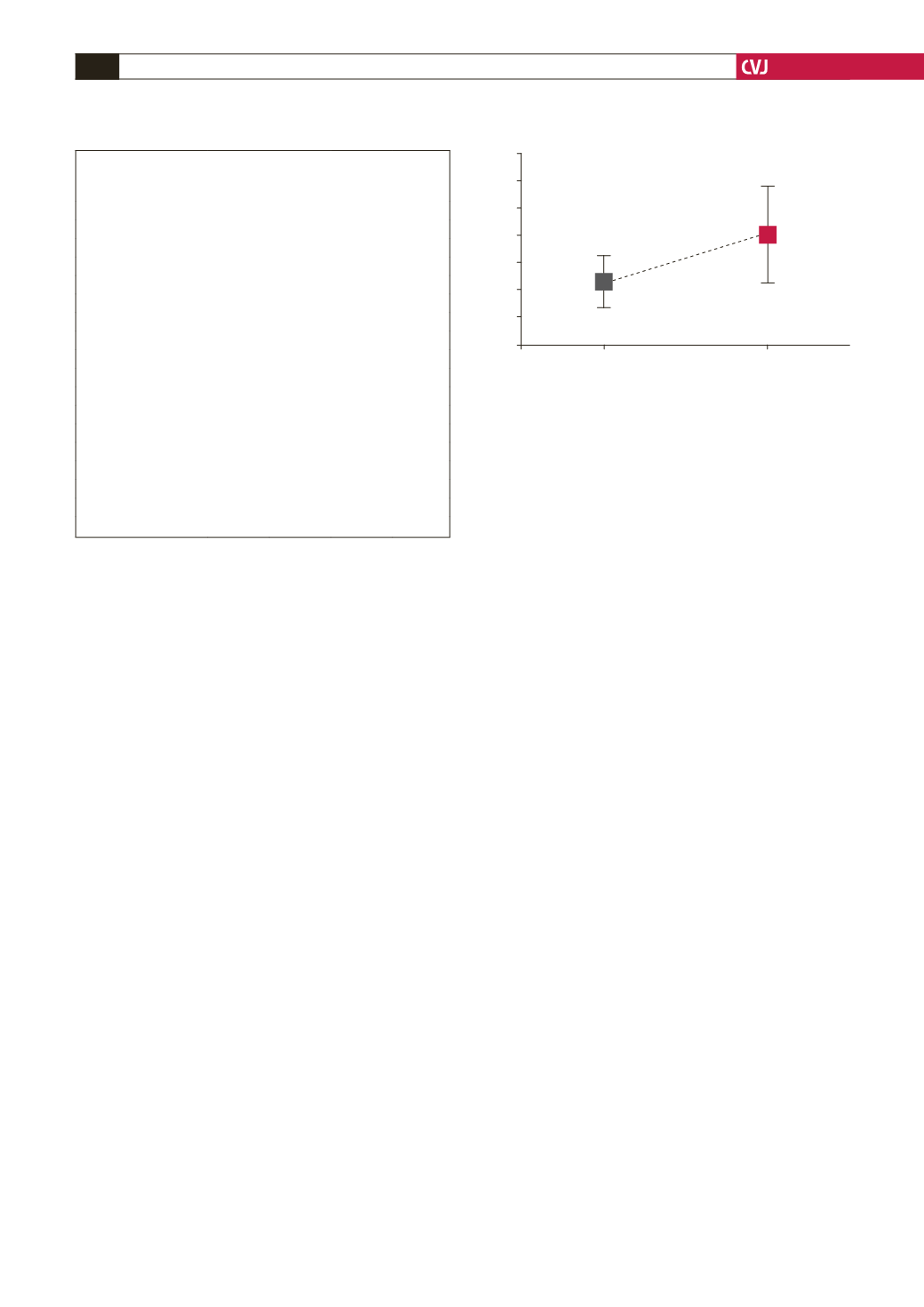
Fig. 5. Mean total serum cholesterol versus QTc interval
for NQTc and LQTc groups of patients.
6.0
5.8
5.6
5.4
5.2
5.0
4.8
4.6
NQTc
LQTc
QTc interval
Total serum cholesterol (mmol/l)
p
=
0.0355
Bar = 95% CI
TABLE 1. ASSOCIATION BETWEEN LQTc AND
NQTc GROUPS OF PATIENTSWITH REGARD
TO MAJOR RISK FACTORS FOR IHD
Risk factor present
Yes,
n
(%)
No,
n
(%)
Total,
n p
-
value
Diabetes mellitus
NQTc
62 (29)
149 (71)
211
0.54
LQTc
29 (33)
59 (67)
88
Total
n
91
208
299
Smoking
NQTc
116 (56)
92 (44)
208
0.19
LQTc
55 (64)
31 (36)
86
Total
n
171
123
294
Hypertension
NQTc
157 (74)
55 (26)
212
0.23
LQTc
70 (80)
17 (20)
87
Total
n
227
72
299
Family history
NQTc
74 (36)
134 (64)
208
0.045*
LQTc
21 (24)
67 (76)
88
Total
n
95
201
296
*
Statistically significant association.