CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 4, July/August 2011
188
AFRICA
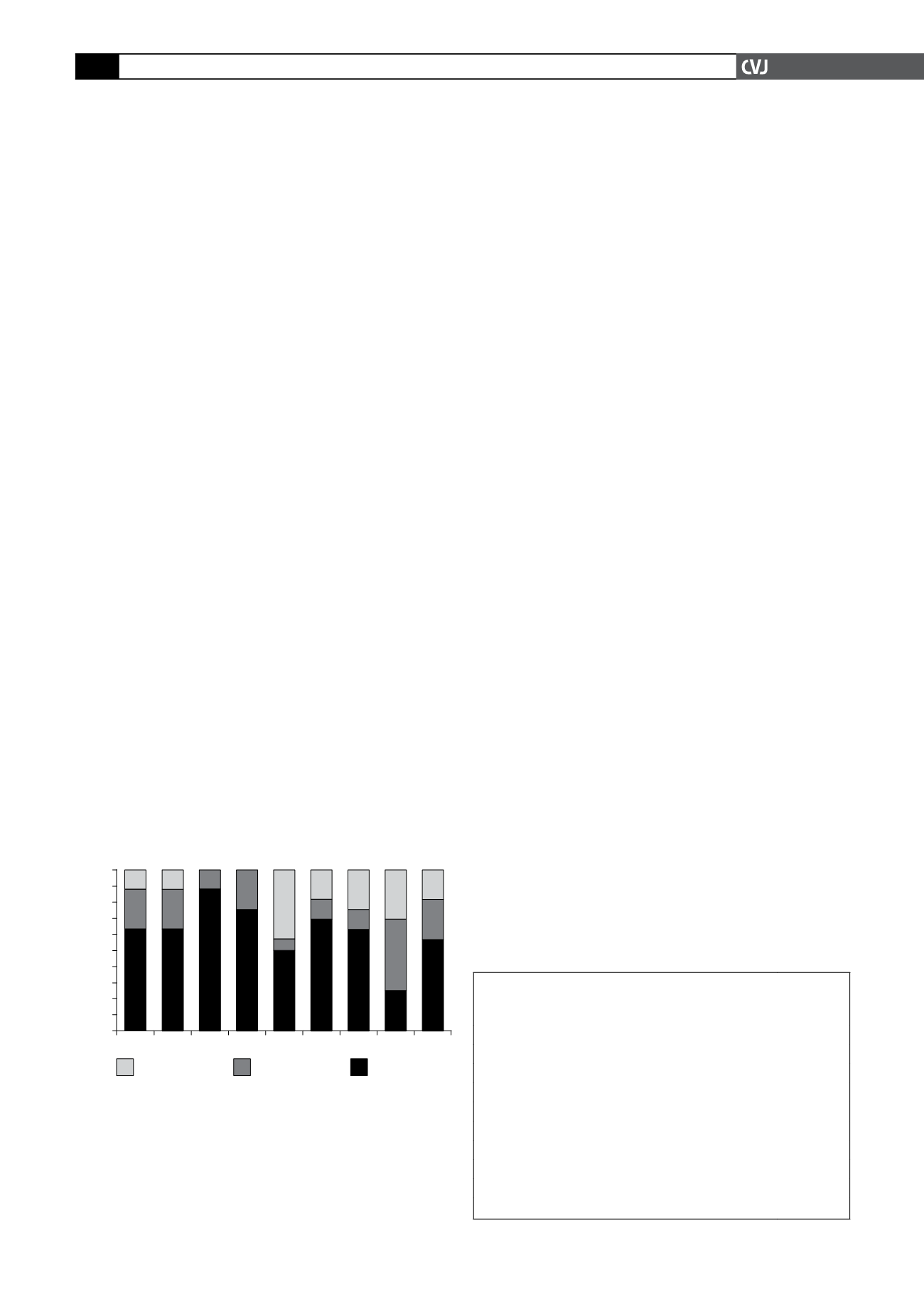
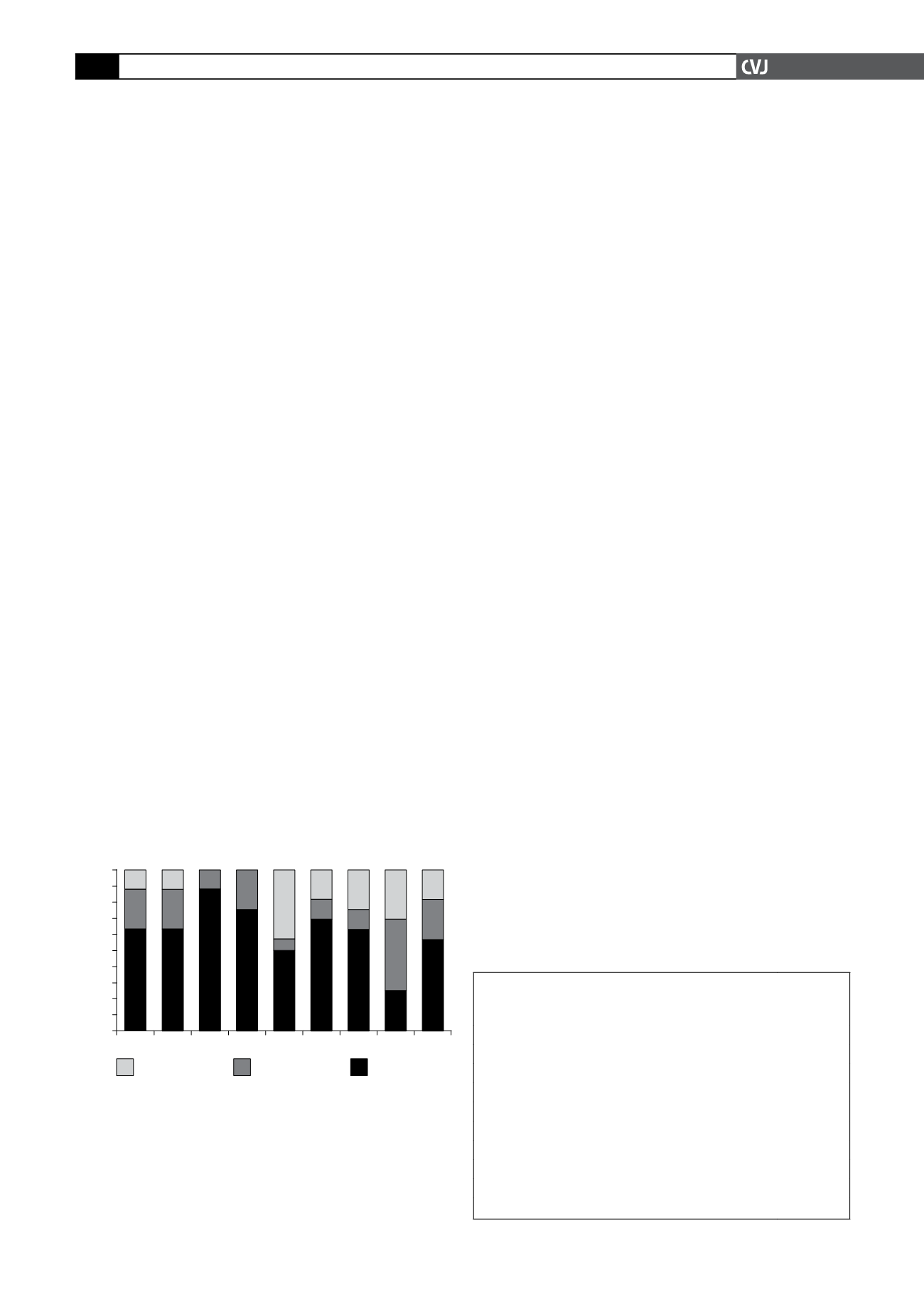
the following compelling indications are present: ischaemic
heart disease or angina, heart failure, diabetes mellitus, prior
cerebrovascular accident, peripheral vascular disease, albumi-
nuria, chronic kidney disease, left ventricular hypertrophy, and
isolated systolic hypertension. Knowledge of the compelling
indications for treatment of hypertension was poor, with the
majority (62.5%) of doctors not knowing what the appropriate
agent of choice for these conditions should be (Fig. 2).
Factors influencing optimal management of
hypertension
The main challenges to optimal treatment of hypertension in their
settings, as reported by doctors in this study, included: (1) poor
patient adherence to prescribed treatment (75%); (2) language
difficulty (50%); (3) overwhelmingly heavy patient load (50%);
(4) significant medical staff shortages (50%); and (4) patient loss
to follow up (44%). Other factors that were mentioned included
conditions of adverse poverty under which many patients live;
poor patient literacy; intermittent shortage or lack of drugs; lack
of functional equipment (including sphygmomanometers); and
other systematic factors (Table 3).
Discussion
The findings of this study suggest that the knowledge of South
African primary healthcare practitioners regarding hypertension
and its management is sub-optimal. Knowledge on the South
African hypertension guidelines is poor. Doctors estimated that
about two-thirds of their hypertensive patients have poor blood
pressure control, and yet treatment for these patients is not
routinely titrated upwards. Moreover, the doctors who participat-
ed in this study identified significant challenges to their effective
management of hypertension.
Various stakeholders in the healthcare sector will have to
work together to address these challenges if we are to improve
care of hypertensive patients in this country. Furthermore, ongo-
ing education of doctors is crucial in order to increase knowledge
on hypertension and awareness of the management guidelines
and to encourage them to overcome physician inertia. On a posi-
tive note, it is interesting to observe that
b
-blockers were not
considered as first-line treatment of hypertension, in the absence
of compelling indications.
Despite hypertension being identified as an important aspect
of the practice of doctors at the primary healthcare level, many
doctors do not focus on lifestyle modifications. The reason for
this phenomenon, as reported by the doctors surveyed, is the
lack of adequate time at each consultation for explanation to
patients about necessary lifestyle changes to complement their
drug treatments.
The sixth report of the Joint National Committee on preven-
tion, detection, evaluation and treatment of high blood pressure
included evidence-based lifestyle modifications that have been
shown to lower blood pressure in normotensive and hypertensive
patients.
7
These important lifestyle modifications include weight
loss of 3 to 9%, moderation in alcohol use, smoking cessation,
increased physical activity, reduced dietary salt intake, reduced
intake of saturated fats and cholesterol, and adequate dietary intake
of potassium, calcium and magnesium. Each of these lifestyle
changes have the effect of lowering systolic blood pressure by 3 to
11 mmHg and the diastolic blood pressure by 2.5 to 5.5 mmHg.
8-12
Therefore, as drugs fail to adequately control blood pressure
in the majority of patients, these lifestyle changes are impor-
tant adjuncts in the initial and comprehensive management of
patients with an elevated blood pressure. These lifestyle altera-
tions should be enforced at the primary level of care, rather than
waiting for patients to develop complications and to receive these
messages from secondary and tertiary hospitals, when they may
be too late.
A disturbing finding was that a significant proportion (37.5%)
of doctors surveyed did not aim to treat patients to target.
Despondency on the part of overwhelmed healthcare practition-
ers, including doctors in the primary level of care within the
public sector in South Africa, in the management of hypertension
has previously been documented by several authors.
7,13,14
The net
effect of these despondent attitudes towards patient care is further
compromising an already crumbling management paradigm.
Almost 90% of doctors in this study were below the age of 40
years, with most having practiced as doctors for 10 years or less.
This observation reflects the state of healthcare in South Africa,
where fairly junior doctors are entrusted with enormous clinical
responsibility. While these young doctors grow quickly in their
trade and benefit from having to assume responsibility for the
TABLE 3. PROPORTION OF DOCTORSWHO IDENTIFIED
FACTORS INFLUENCING OPTIMAL MANAGEMENT OF
HYPERTENSION
Poor patient treatment adherence
12 (75.0)
Language difficulty
8 (50.0)
Overwhelming patient load
8 (50.0)
Severe staff shortages
8 (50.0)
Patient loss to follow up
7 (43.75)
Poverty
4 (25.0)
Poor patient literacy
3 (18.75)
Lack of drugs
2 (12.5)
Lack of functional equipment
2 (12.5)
Systematic factors like financial constraints on tests
3 (18.75)
Angina PMI
HF DM CVA Alb CKD LVH JISH
Fig. 2. Choice of preferred antihypertensive agent, when
these compelling indications are present. Angina
=
ischaemic heart disease or angina pectoris, PMI
=
previ-
ous myocardial infarct, HF
=
heart failure, DM
=
diabetes
mellitus, CVA
=
prior cerebrovascular accident, PVD
=
peripheral vascular disease, Alb
=
albuminuria, CKD
=
chronic kidney disease, LVH
=
left ventricular hypertro-
phy, and JISH
=
just isolated systolic hypertension.
100
90
80
70
60
50
40
30
20
10
0
unknown
incorrect
correct
Indications for treatment of hypertension
Choice of treatment (%)