CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 4, July/August 2014
AFRICA
187
with stable CAD.
21
The presence of a reversible perfusion deficit
is associated with a tripled risk for death or non-fatal myocardial
infarction.
22
The presence of abnormal CMR characteristics,
including a reversible perfusion deficit, is a strong predictor of
myocardial events during follow up.
23
Viability assessment
Several different methods of assessing myocardial viability
are available in the diagnostic armamentarium. Viability tests
have become a crucial tool in evaluating whether patients with
congestive cardiac failure related to CAD might benefit from
revascularisation therapy.
24-26
Allman
et al
.
27
demonstrated a strong association between
viable myocardium on non-invasive testing and increased survival
after revascularisation, with a reduction in annual mortality of
79.6% compared with medical therapy. Three CMR methods
exist for the evaluation of viability:
•
resting LV wall end-diastolic wall thickness (
>
5 mm regarded
as viable)
28
•
low-dose dobutamine (LDD) stress assessment of contractile
reserve
29
•
LGE of non-viable scar tissue.
30
According to a recent meta-analysis, LGE CMR provides the
highest sensitivity and negative predictive value among the
three methods. LDD CMR, however, has the highest specificity
and PPV.
31
If LGE CMR is compared with PET-FDG, rest-
distribution thallium-201 SPECT and technetium-99m
sestamibi-SPECT, and dobutamine stress echocardiography, it
also performs better for predicting functional improvement after
revascularisation of hibernating myocardium. LGE CMR also
has a higher sensitivity, NPV and PPV than the other available
techniques.
25,32
Cardiovascular MRI provides a unique tool to assess multiple
interrelated clinical markers of viability in a single test.
29
The
comprehensive assessment of ventricular mass, volume, function
and perfusion as well as the ability to establish the presence and
extent of non-viable tissue and AAR during a single CMR scan is
unparalleled in the diagnostic work-flow of ischaemic heart disease.
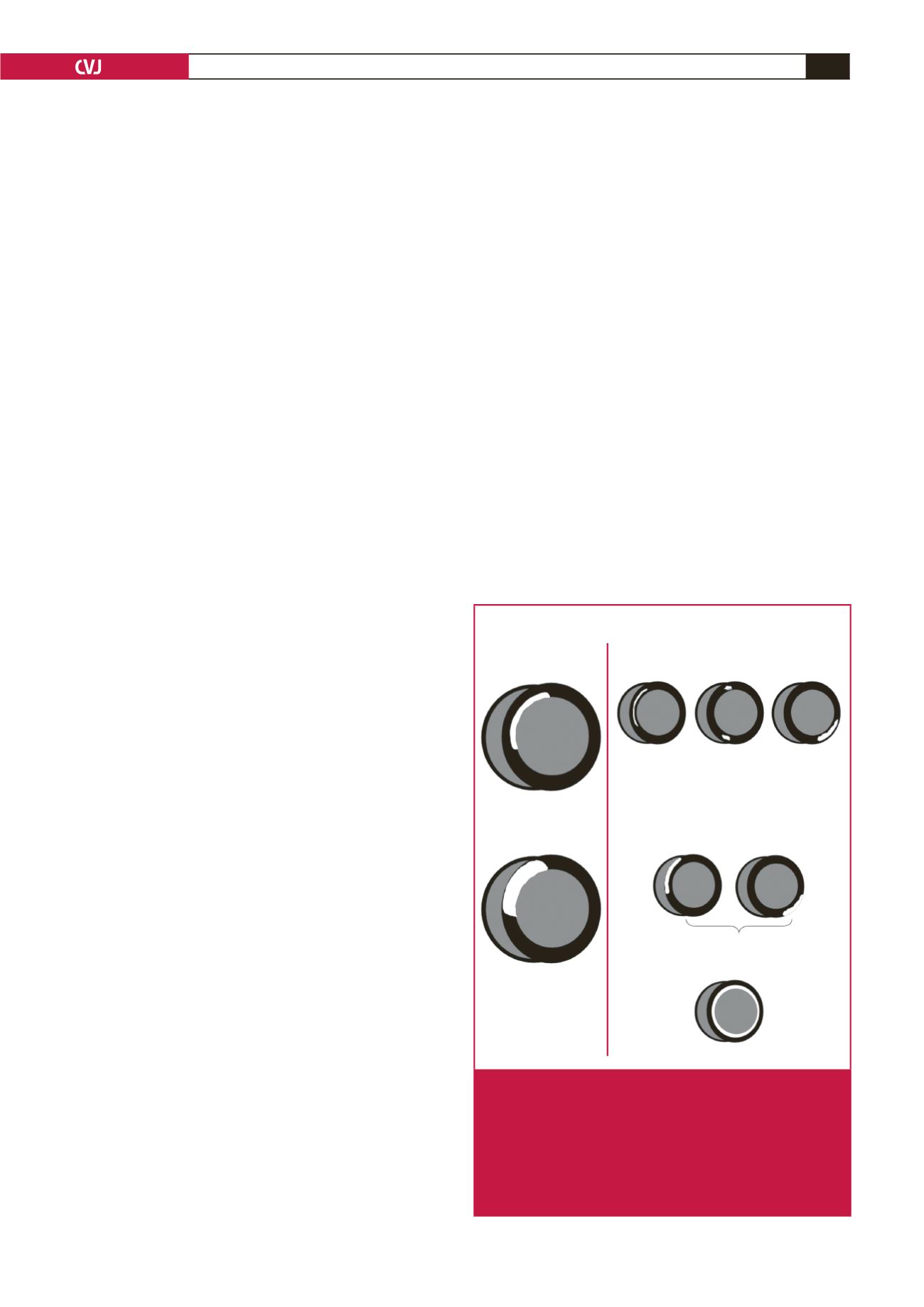
Cardiomyopathies
CMR is fast becoming an invaluable tool in the assessment of
cardiomyopathies. Regional and global myocardial function can
be assessed, and its unique capability to visualise the apex and
lateral wall supersedes all other imaging modalities. It is also
unique in being able to perform tissue characterisation and to
suppress fat, which, combined with LGE, assists in differentiating
between various forms of cardiomyopathy (Fig. 2).
Hypertrophic cardiomyopathy (HCM) is the leading cause of
sudden death in young people. The majority of HCM patients
with sudden cardiac death have few or no clinical symptoms.
33
CMR is a powerful tool in the diagnosis and risk stratification of
HCM; it is widely accepted as the gold standard for assessment
of myocardial function as well as left ventricular mass, which
has been shown to be a sensitive predictor of adverse outcomes
in HCM.
34
According to a recent meta-analysis, the presence of LGE
can predict a higher risk for sudden cardiac death (SCD) and
heart failure in patients with HCM, thereby identifying patients
who would benefit from ICD placement.
35
The presence of
oedema on T2-weighted CMR has also been observed in
patients with HCM.
36
The presence of LGE has been shown to
be a marker for adverse outcomes in several other non-ischaemic
cardiomyopathies.
37,38
LGE CMR can help to differentiate
between ischaemic and non-ischaemic dilative cardiomyopathy.
39
According to the revised Task Force criteria for arrhythmogenic
right ventricular dysplasia published in
Circulation
in 2010, MRI
findings now fall under the major and minor criteria.
40
Albeit non-specific, CMR findings in ARVD include fatty
infiltration of the RV wall, dilatation of the RV, regional or
global RV dyskinesis and patchy areas of LGE in the RV
wall mainly. CMR shows a characteristic pattern of global
sub-endocardiallate enhancement as well as abnormal myocardial
and blood-pool kinetics in patients with cardiac amyloidosis.
41
CMR is a useful diagnostic tool in cardiac involvement owing
to sarcoidosis, which is responsible for the majority of deaths
resulting from sarcoidosis.
42,43
Myocarditis
Endomyocardial biopsy (EMB) is considered to be the gold
standard for the diagnosis of myocarditis. Recently, CMR has
emerged as a promising non-invasive alternative. Three CMR
techniques are applied in myocarditis:
Hyperenhancement patterns
Ischaemic
A. Subendocardial Infarct
A. Mid-wall HE
B. Epicardial HE
•Idiopathic Dilated
Cardiomyopathy
•Myocarditis
•Hypertrophic
Cardiomyopathy
•Right ventricular
pressure overload
(e.g. congenital
heart disease,
pulmonary HTN)
•Sarcoidosis
•Myocarditis
•Anderson-Fabry
•Chagas Disease
C. Global Endocardial HE
B. Transmural Infarct
Non-ischaemic
•Sarcoidosis, Myocarditis, Anderson-Fabry, Chagas Disease
•Amyloidosis, Systemic Slcerosis, Post cardiac transplatation
Fig. 2.
Hyper-enhancement patterns that one may encounter
in clinical practice. If hyper-enhancement is present,
the endocardium should be involved in patients with
ischaemic disease. Isolated mid-wall or epicardial
hyper-enhancement strongly suggests a ‘non-ischae-
mic’ aetiology. (Reprinted with permission from Shah
et al. Clinical Magnetic Resonance Imaging, 3rd edn.
New York: Elsevier Press; 2005.)