CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 1, January/February 2011
6
AFRICA
Editorial
Maternal mortality
Issues surrounding maternal mortality have recently been widely
published in both the lay media and the health fraternity litera-
ture. Possible reasons for this are that there are only five years
remaining until the 2015 deadline to have achieved the United
Nations Millennium Development Goals (MDGs). The general
impression among health professionals is that there has been
slow progress in achieving MDG 5 (maternal health), which
targets a three-quarters reduction in maternal deaths from 1990–
2015. There have, however, been two recent publications, which
are reflective of slow but significant progress in the reduction
of maternal mortality in both high- and low-income countries.
1,2
Last year, Hogan
et al
., using sophisticated mathematical
models, estimated a total of 342 900 maternal deaths for 2008
in 181 countries, and a 1.8% rate of annual decline in mortality
between 1990 and 2008. The authors showed a decline in mater-
nal mortality ratios (MMRs) in both high- and low-income coun-
tries, except for some countries in sub-Saharan Africa and Asia.
1
In the latter part of 2010, the World Health Organisation, the
United Nations Population Fund, the United Nations Children’s
Fund and the World Bank issued the latest estimates on global
MMRs. According to these estimates presented for 171 coun-
tries, approximately 358 000 deaths occurred worldwide in
2008.
2
The global maternal mortality ratio fell by 34%, with
the biggest reductions occurring in eastern Asia and northern
Africa (63 and 59%, respectively). It should be noted however,
that the levels and trends varied widely within regions. Although
there was a decline in some African countries, South Africa,
Botswana, Swaziland, Kenya and Zimbabwe were estimated
to have increased MMRs. The possible reason for the lack of
reduction or increase in MMRs in these countries is probably the
impact of HIV/AIDS.
Overall, it was estimated that in 2008 there were 42 000 deaths
among pregnant women due to HIV/AIDS.
2
In South Africa, the
Saving Mothers report 2005–2007 indicated that non-pregnancy
infections (mainly HIV/AIDS) are the commonest causes of
maternal mortality.
3
The other major causes of maternal deaths
in South Africa are shown in Table 1. Hypertensive disorders of
pregnancy are the commonest direct causes of maternal mortal-
ity. Poorly controlled pre-eclampsia (both in the intra- and post-
partum periods) are common avoidable factors.
Besides HIV/AIDS, hypertensive disorders and obstetric
haemorrhage, which are major causes of maternal deaths, some
mothers are diagnosed to have medical conditions such as cardiac
disease for the first time only in pregnancy. Detection of cardiac
disease, cardiomyopathy, control of hypertension and diabetes,
with proper advice on family planning, may help decrease mortal-
ity andmortality associated withmedical conditions in pregnancy.
Maternal mortality is also impacted on by racial disparities.
Bryant
et al
. have shown that African-American mothers have
a three- to four-fold higher mortality than other major racial or
ethnic groups in the USA, and propose a five-domain framework
to identify contributors, namely, behaviour patterns, genetic
predisposition, social circumstances, environmental exposures
and shortfalls in medical care. They found that social circum-
stances and medical care were the most important factors.
4
Therefore, interventions to reduce maternal mortality must
address social determinants of health besides focusing on
reducing obstetric haemorrhage by improving care in labour
and delivery, reducing venous thrombo-embolism with DVT
thrombophylaxis, reducing deaths from cardiac disease with
education for earlier recognition, and effective multi-disciplinary
care. Access to care, particularly longitudinal care for women
with underlying medical conditions, is a critical issue and should
become a part of the care provided by all working in the field of
cardiovascular medicine.
J MOODLEY, MB, ChB,
For the National Committee on Confidential Enquiries into
Maternal Deaths, National Department of Health, South Africa
Women’s Health and HIV Research Group, Nelson R Mandela
School of Medicine, University of KwaZulu-Natal, South Africa
References
1. Hogan MC, Foreman KJ, Naghavi M,
et al
. Maternal mortality for
181 countries, 1980–2008: a systematic analysis of progress towards
Millennium Development Goal 5.
Lancet
2010;
375
: 1609–1623.
2. Wilmoth J, Mathers C, Say L, Mills S. Maternal deaths drop by one-third
from 1999–2008: a United Nations analysis.
Bull Wld Hlth Org
2010;
88
: 718–718A.
3. National Committee on Confidential Enquiries into Maternal Deaths.
Saving Mothers. Fourth Report on Confidential Enquiries into Maternal
Deaths in SouthAfrica 2005–2007. Department of Health, Pretoria. 2009.
4. Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic
disparities in obstetric outcomes and care: prevalence and determinants.
Am J Obstet Gynecol
2010;
202
: 335–343.
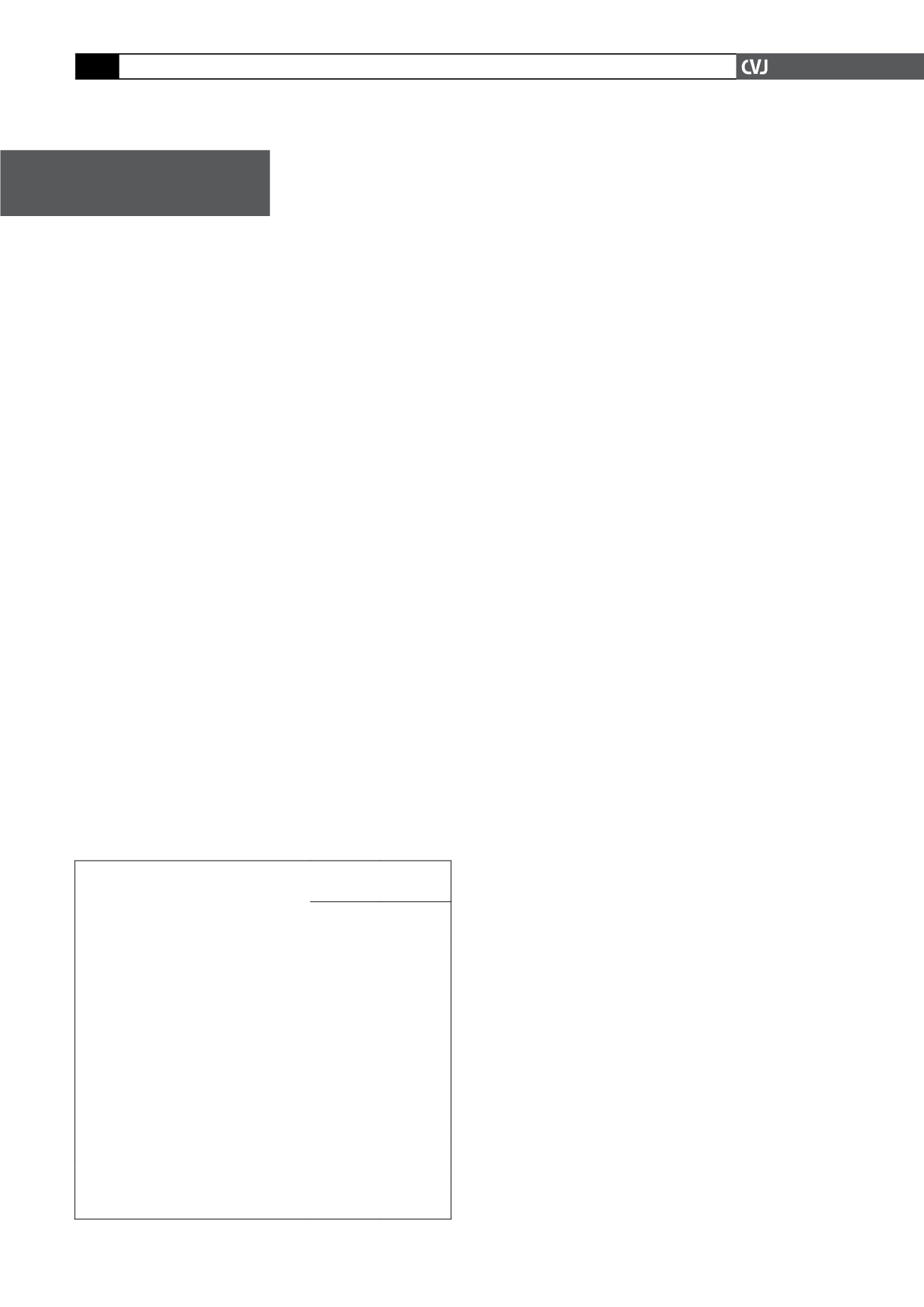
TABLE 1. PRIMARY OBSTETRIC CAUSES OF MATERNAL DEATHS
Primary Obstetric Cause
2005–2007
N
%
Direct
1819
45.9
Hypertension
622
15.7
Postpartum haemorrhage
383
9.7
Antepartum haemorrhage
108
2.7
Ectopic pregnancy
55
1.4
Abortion
136
3.4
Pregnancy-related sepsis
223
5.6
Anaesthetic related
107
2.7
Embolism
57
1.4
Acute collapse
128
3.2
Indirect
1966
49.7
Non-pregnancy-related infections
1729
43.7
AIDS
915
23.1
Pre-existing maternal disease
237
6.0
Unknown
174
4.4
Coincidental
118