CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 9, October 2012
AFRICA
e5
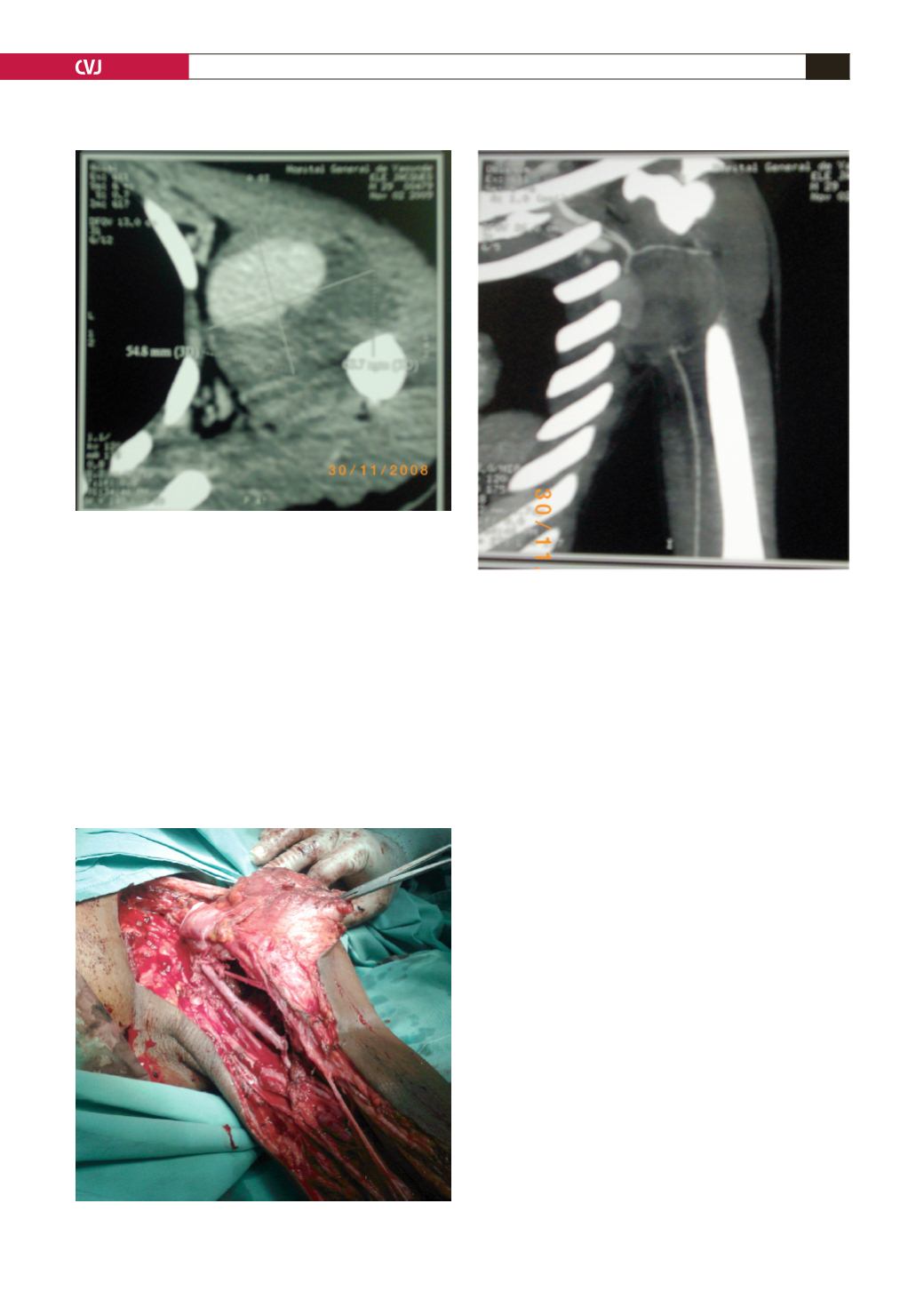
in diameter, involving the second and third segments of the AA.
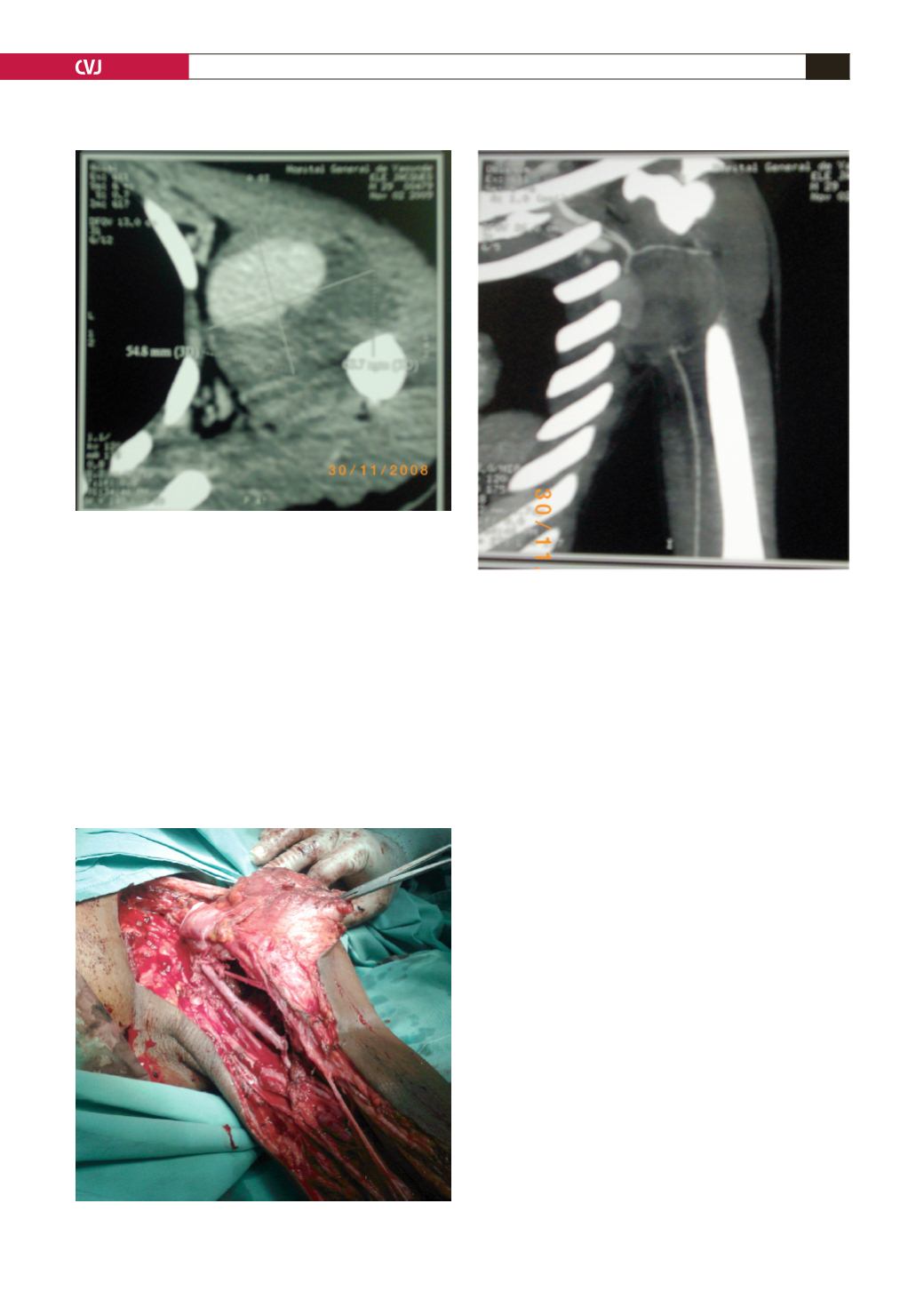
The humeral artery was patent (Figs 2, 3). Electromyography
revealed diffuse brachial plexus lesions corresponding to the C5,
C6 and C8 roots. The pre-operative work-up showed no other
abnormality.
Conventional surgical treatment was decided on, with exeresis
of the aneurysm, brachial plexus liberation and axillo-humeral
bypass with a vein. Under general anaesthesia, the patient was
placed in a supine position, with the shoulder slightly elevated
and the arm in a horizontal position, forming a 90º angle with
the body.
Exposure of the left AA was achieved proximally using an
infraclavicular approach and distally using the classic humeral
approach. A prolongation in the delto-pectoral groove was
performed to divide the pectoralis major and transect the
pectoralis minor. The large pseudoaneurysm was identified.
Before the 45-min clamping, 5 000 IU heparin sulfate was
administered intravenously. A total exeresis of the aneurysm
was performed and a mild brachial plexus laceration was found.
A 12-cm saphenous vein interposition was done using a 5-0
polypropylene (Fig. 4).
The postoperative period was uneventful. The intervention
site and the patency of the AA were evaluated clinically and with
ultrasound daily until discharge (eight days), then weekly for one
month, monthly for one trimester, and subsequently every six
months. Physiotherapy and six-month oral anticoagulation were
recommended after discharge.
To date, two and half years after the surgery, on ultrasound the
AA is patent without stenosis or enlargement. The neurological
deficit has improved and the patient has resumed duty with the
affected limb.
Discussion
Epidemiology
Axillary artery peudoaneurysms are rare and the published
experience is limited to around five cases reported in the last
20
years, as determined from a Medline search of the literature.
The aetiologies are post-traumatic, severe or recurrent anterior
shoulder dislocation,
2-6
and humeral head fractures.
7,8
Blunt
arterial injuries of the shoulder account for only 5% of all arterial
injuries in this area, whereas penetrating wounds, as was the case
here, are more frequent, representing 95%.
8
Fortunately, false aneurysms secondary to penetrating wounds
have not been reported. This is probably due to the fact that
vascular wounds are easy to discover and manage immediately,
Fig. 2. CTA demonstrating the axillary artery pseudo-
aneurysm.
Fig. 3. Axillary artery pseudoaneurysm demonstrating
the patency of the humeral artery.
Fig. 4. Surgical view of the saphenous vein graft (arrow).