CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 2, March 2013
20
AFRICA
warfarin.
22
In addition, drugs such as NSAIDs that possess
antiplatelet activity can produce additive anticoagulant effects on
concurrent administration with warfarin.
23
Broad-spectrum antibacterial agents, through their effects
on the vitamin K-producing gut flora, increase the effect
of warfarin.
24
Competitive substrates, inducers and inhibitors
of CYP2C9 and CYP3A4 can alter warfarin plasma levels,
with consequent alterations in INR.
25
Therefore studies on
utilisation and responses of warfarin in different patient groups
are important to assess the causes of differences in its clinical
response in a specific environment.
In South Africa, primary healthcare anticoagulation clinics
play an essential role in warfarin therapy. These clinics are
responsible for the education, optimisation and maintenance
of anticoagulant therapy in referred patients. The initiation
of anticoagulation is usually performed by the referring
doctor following appropriate diagnosis and indications. The
anticoagulant clinics are responsible for ensuring there are no
contraindications to warfarin therapy (especially the presence of
severe bleeding, first and third trimester pregnancy, and severe
hepatic disorders) and ascertaining compliance to therapy.
The aim of the present study was therefore to evaluate
warfarin utilisation in two primary-care anticoagulation clinics
in Cape Town, Western Cape, South Africa. The study aimed at
retrospective assessment of INR monitoring with consideration
of possible influences of co-medication on therapy.
Methods
A retrospective study was undertaken of all warfarin-related
prescriptions in the warfarin clinics of Wesfleur and Gugulethu
hospitals, covering a 12-month period between June 2008 and
May 2009. Wesfleur Hospital is located in Atlantis, an area
under the West Coast district municipality with a population
of about 140 000 people, the majority being Coloured [the
race classification was based on the national census categories,
and described as black (Africans), Coloured, Indian and
white]. It is a level-two facility which sees an average of
13 000 patients monthly. It runs a warfarin clinic every Friday,
managed by a doctor and supported by specialist physicians at
New Somerset Hospital, Cape Town, for referrals.
Gugulethu Hospital is situated in the highly populated
Gugulethu Township in the City of Cape Town municipality, and
is inhabited primarily by blacks. The hospital takes care of about
6 800 patients per month. The warfarin clinic is mostly managed
by a nursing sister or staff nurse, who contacts a doctor if the
patient’s INR results are abnormal.
Data extracted from the patient folders included age,
gender, race, weight, address, concurrent chronic illnesses and
medication, INR history (monthly INR levels measured in
the 12-month period of the study) and indication for warfarin
therapy. For the purpose of this study, a cut-off INR level of 3.5
was chosen. Patients above this limit have an increased risk of
toxicity, as discussed above. Patients were assigned to the INR >
3.5 group if they had one or more INR levels above 3.5 during
the course of the study.
Medications taken concurrently were pre-classified as
potentially relevant or non-relevant for drug–drug interactions
with warfarin using the South African Medicines Formulary
(SAMF). A list of drugs taken concurrently that could result in
drug–drug interactions was compiled.
Ethics approval for the project was obtained from the Health
Research Ethics Committee of the University of Stellenbosch,
and Wesfleur and Gugulethu Hospital managements approved
this project.
MS Excel was used to capture the data and STATISTICA
version 8 (data analysis software system,
www.statsoft.com)(StatSoft Inc, 2008) was used for data analysis. Summary
statistics was used to describe the variables. The Chi-square test
was used for statistical comparison between groups. A
p
-value
<
0.05 represented statistical significance in hypothesis testing.
Results
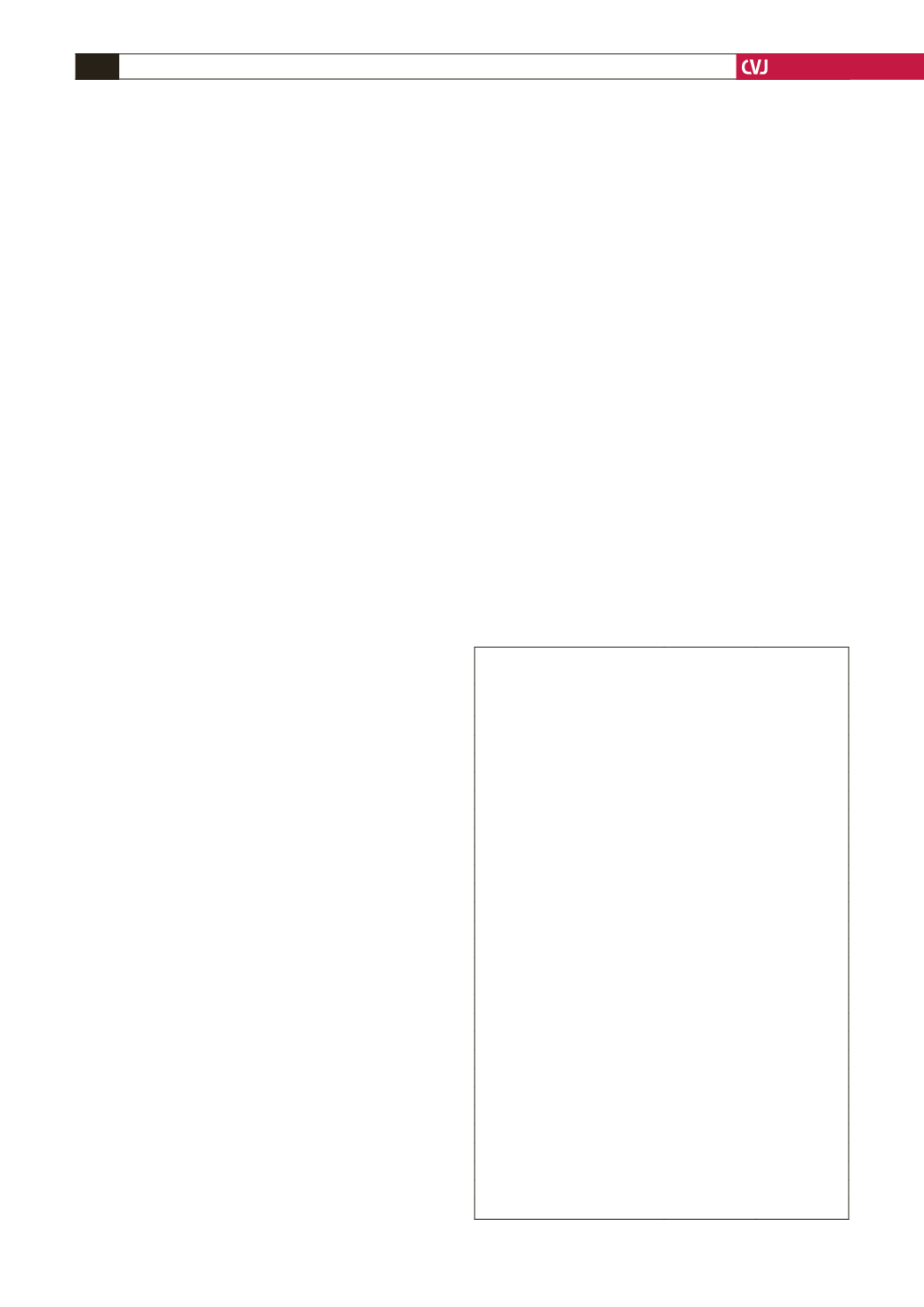
A total of 111 patient folders were retrieved and qualified
for this study after the exclusion of eight (four from each
hospital) due to incomplete data. The demographic variables
are summarised in Table 1. The Wesfleur Hospital had more
patients (76) on anticoagulant therapy than Gugulethu (35). The
racial distribution of the patients reflected the demography of
the inhabitants in the hospital locations; 88.1% of the patients
in Wesfleur were Coloured while all patients from Gugulethu
were black.
There was a significant variation in INR records in both
hospitals. While none of the patient records showed an INR
less than 2, over a third of the patients (32.2%) had at least one
record of INR greater than 3.5 in Gugulethu Hospital, compared
TABLE 1. DEMOGRAPHICAND INRVALUES FOR PATIENTS
FROMWESFLEURAND GUGULETHU HOSPITALS
Wesfleur
(
n
=
76)
Gugulethu
(
n
=
35)
Gender
Male
37.5
19.4
Female
62.5
80.6
Race
Black
5.3
100
White
5.3
0
Coloured
88.1
0
Unspecified race
1.3
0
Co-morbidities
Diabetes
13
23
Hypertension
61
58
Arthritis
16
14
Chronic obstructive airway disease
11
6
Peptic ulcers
8
3
INR values
INR
>
3.5
58.3
32.2
Gender vs INR
Male: INR
>
3.5
51.9 (
n
=
27)
50 (
n
=
6)
Female: INR
>
3.5
62.2 (
n
=
45)
28 (
n
=
25)
Age vs INR
Patients
>
40 years
86.1
58.1
Patients
>
40 years: INR
>
3.5
59.7 (
n
=
62)
33 (
n
=
18)
Patients
<
40 years: INR
>
3.5
40 (
n
=
10)
23 (
n
=
13)
Weight vs INR
Patients
>
70 kg
33.7
82.4
Patients
>
70 kg: INR
>
3.5
72 (
n
=
32)
35.7 (
n
=
14)
Patients
<
70 kg: INR
>
3.5
55 (
n
=
31)
33.3 (
n
=
3)



















