CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 1, January/February 2014
AFRICA
37
(
p
=
0.05,
R
2
=
0.11). However, in multivariate regression, LAA,
Tei index and Ea remained in the model to predict LVEDP (
p
=
0.02,
R
2
=
0.26). This model (Table 2) had an area under the ROC
curve of 0.71 (95% CI: 0.61–0.80).
We then dichotomised the LVEDP as below 15 and above 15
mmHg. In our series of patients, six had LVEDP
≥
15 mmHg
and the remaining 27 had values below 15 mmHg. The best
model for predicting this variable consisted of LAA, IVRT and
Ea. The results of univariate and multivariate logistic regression
for predicting dichotomised LVEDP (
<
15 vs
≥
15 mmHg) are
presented in Table 3.
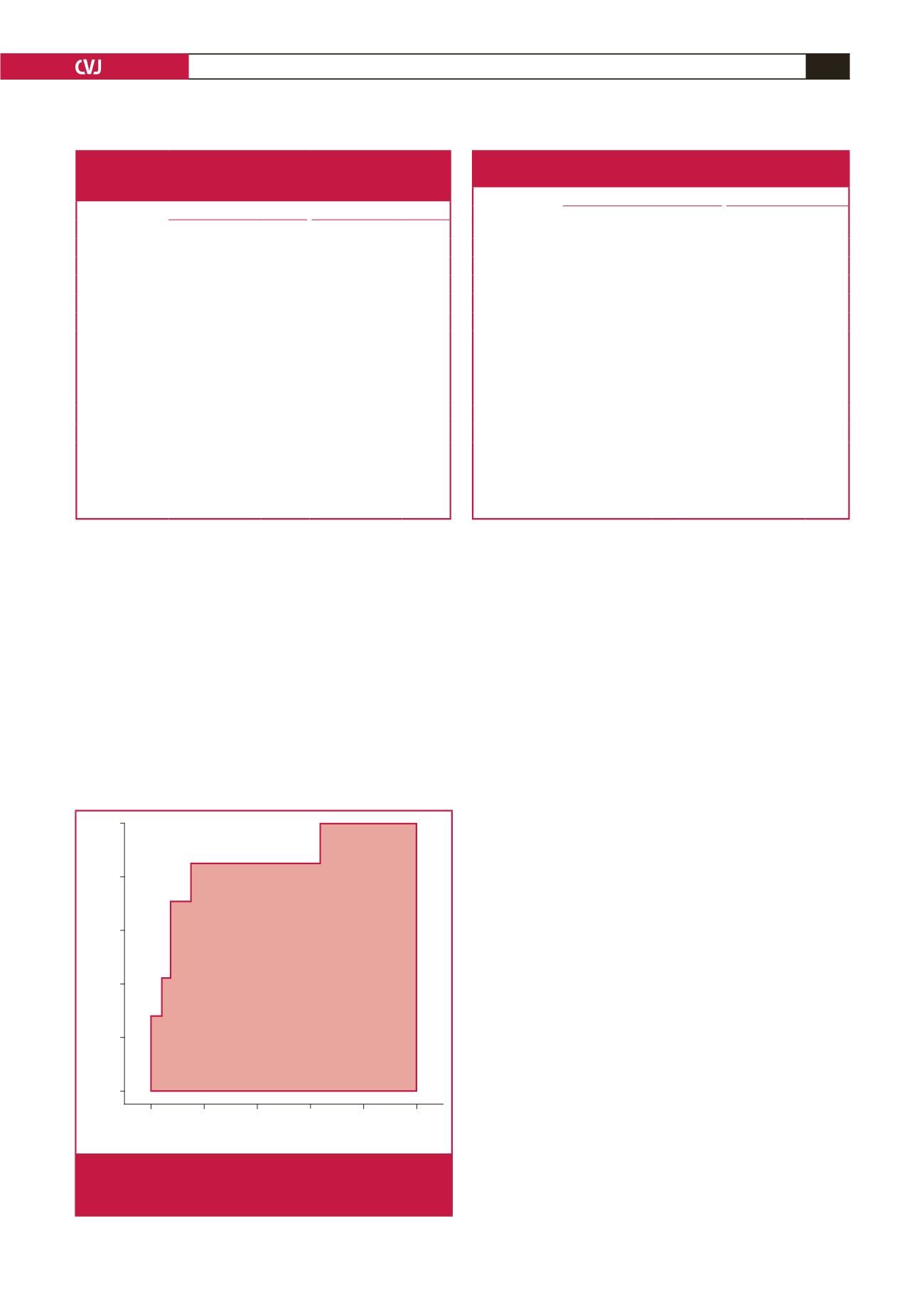
For prediction of a mean LVEDP
≥
15 mmHg and with the
use of ROC curves, the model had a sensitivity of 85% and
a specificity of 85% (Fig. 2). This sensitivity and specificity
corresponded to the model value of –1.584. The area under the
ROC curve was 0.86 (95% CI: 0.7–1;
p
<
0.001).
The LAP for the 29 patients was 21.6
±
8.9 mmHg and
ranged from 8 to 50 mmHg. In univariate analysis, significant
relationships were noted between E/Ea (
p
=
0.005,
r
2
=
0.22),
E/VP (
p
=
0.032,
r
2
=
0.13), LAA (
p
=
0.013,
r
2
=
0.175) and
PVs/PVs
+
PVd (
p
=
0.006,
r
2
=
0.21). In multivariate analysis
E/Ea, LAA and PVs/PVs
+
PVd remained in the model to predict
LAP (
p
=
0.001,
r
2
=
0.39). The results of the univariate and
multivariate analyses are presented in Table 4.
Discussion
The present study showed that conventional parameters of LV
diastolic function are of limited value in patients with MS.
However, it supported a model to estimate LVEDP in patients
with significant MS. Interestingly, a number of patients with
significant MS had a LVEDP
>
15 mmHg, emphasising the
importance of assessment of LVEDP in this patient population.
Previous studies have reported on the estimation of mean
pulmonary capillary wedge pressure (PCWP) by using
mitral inflow in patients with MR,
13,14
and in those with atrial
fibrillation.
4,15
In only one study,
16
patients with MS were
included. This study reported weak relationships between PCWP
and mitral inflow velocities in patients with MVD, including
patients with MS.
In our study, in patients with MS (with and without AF), there
were no associations between mitral inflow velocities (E, A, E/A,
PHT) and LVEDP or mean LAP. This finding was expected,
given the confounding effects of LV relaxation, LV stiffness,
LAP and MVA on these measurements.
17
Patients with MS have
a prolonged DT despite an elevated LAP due to valvular stenosis,
and DT (or PHT) itself can be used to grade the severity of
MS.
1
It is therefore not surprising that estimation of LV filling
pressure from mitral peak diastolic velocities and DT in patients
Table 3. The results of univariate and multivariate logistic
regression for predicting dichotomised lvedp
(
<
15 vs
≥
15 mmHg)
Univariate model
Multivariate model
Characteristic Coefficient (SE)
p
-value Coefficient (SE)
p
-value
Intercept
–
–
3.66 (6.25)
0.55
IVRT
–0.09 (0.05)
0.05 –0.16 (0.10)
0.12
LAA
0.20 (0.11)
0.06
0.25 (0.13)
0.06
Ea
–0.39 (0.27)
0.15 –0.62 (0.35)
0.07
Tei index
2.70 (3.88)
0.49
E/Ea
3.76 (2.60)
0.41
IVRT/TE–Ea
0.10 (0.14)
0.47
TE–Ea
0.01 (0.01)
0.41
VP
0.02 (0.03)
0.50
E/VP
31.67 (46.45)
0.50
PVs/PVs + PVd –4.06 (5.54)
0.46
SE, standard error; IVRT, isovolumic relaxation time; LAA, left atrium
area; Ea, peak early diastolic velocity of mitral annulus; E, mitral inflow
peak early diastolic velocity; TE–Ea, interval between the onset of mitral
E and annular Ea; VP, mitral inflow propagation velocity, PVs, pulmonary
vein systolic flow velocity; PVd, pulmonary vein diastolic flow velocity.
Table 4. The results of univariate and multivariate analysis for
prediction of the mean lap
Univariate model
Multivariate model
Characteristic
Coefficient
(SE)
R
2
p
-value
Coefficient
(SE)
p
-value
Intercept
–
– – 20.77 (13.92) 0.14
E/Ea
26.40(8.78)
0.22 0.01 17.55 (8.60)
0.05
LAA
0.70 (0.50) 0.17 0.01 0.45 (0.25)
0.08
PVs/PVs + PVd –52.63 (17.92) 0.21 0.01 –32.57 (17.63) 0.07
Ea
–0.87 (0.76) 0.03 0.25
IVRT/TE–Ea
0.15 (0.44) 0.01 0.73
TE–Ea
0.01 (0.03) 0.01 0.55
VP
–0.02 (0.11) 0.01 0.79
IVRT
–0.12 (0.15) 0.02 0.42
E/VP
364.07 (162.38) 0.14 0.03
Tei index
–4.67 (13.36) 0.01 0.73
SE, standard error; E, mitral inflow peak early diastolic velocity; Ea, peak
early diastolic velocity of mitral annulus; LAA, left atrium area; PVs,
pulmonary vein systolic flow velocity; PVd, pulmonary vein diastolic flow
velocity; IVRT, isovolumic relaxation time; TE–Ea, interval between the
onset of mitral E and annular Ea; VP, mitral inflow propagation velocity.
1.0
0.8
0.6
0.4
0.2
0.0
1.0
0.8
0.6
0.4
0.2
0.0
Specificity
Sensitivity
–1.584 (0.852, 0.857)
AUC: 0.862
Fig. 2.
Receiver operating characteristics (ROC) curve of the
developed model for predicting mean LVEDP
≥
15
mmHg. AUC: area under the curve.