
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 4, July/August 2015
e16
AFRICA
appearance of a haematoma at the proximal part of the aortic
arch and a flap entering into the aorta from the aortic arch
during ventricular diastole. Mild aortic valve regurgitation due
to dilation was confirmed.
A filling defect had been determined at the level of the aortic
arch on the angiography performed in another centre. It was
learned that the angiography could not be continued since the
catheter had been placed into the false lumen. Considering the
poor condition of the patient and the possibility of rupture of
the dissection, she was operated on emergently.
Surgical treatment
A median sternotomy was performed under general anaesthesia.
Arterial cannulation was performed through a 10-mm graft
anastomosed to the right subclavian artery in an end-to-
side fashion. Venous cannulation was performed through the
right atrium and cardiopulmonary bypass was established. Left
ventricular decompression was achieved through the right upper
pulmonary vein.
Total circulatory arrest (TCA) was established by reducing
the temperature to approximately 18°C. Iced saline was applied
around the patient’s head for brain protection. Cerebrovascular
circulation was established by administering one-fifth of the
total cardiac output to the right carotid artery through the right
subclavian artery during circulatory arrest. Coronary perfusion
was established with antegrade blood cardioplegia.
The ascending aorta was opened in an oblique fashion. It was
observed that the intimal layer of the ascending aorta caused
an obstruction by prolapsing into the aortic arch (Fig. 2). A
definitive diagnosis was made by observation of the prolapse
of the circumferential dissection flap into the aortic arch. The
prolapsed intimal layer flap was resected through the aortic arch.
The coronary ostia were seen to be open and retrograde flows
were sufficient in the aortic arch.
The distal part of the ascending aorta was constructed using
a 30-mm Dacron graft (Gorotex
®
) with a continuous suture
technique. The posterior part of the anastomosis was supported
with single-pledget mattress sutures. After draining the air
bubbles in the artery, the ascending aorta was cross-clamped
to the new vascular graft and cardiopulmonary bypass was
established. Deep hypothermia was terminated. TCA lasted
13 minutes. The function and structure of the aortic valve and
coronary ostia were normal.
Fibrin glue was used to adhere the dissection flap at the
proximal anastomosis site of the graft in the supracoronary
region. The flap was sutured over itself with a continuous suture
technique. The Dacron graft (Gorotex
®
) was anastomosed to
the supracoronary aorta with a continuous suture technique.
The posterior part of the anastomosis was supported with
pledget mattress sutures. The aortic cross-clamp was terminated
after draining the air bubbles in the heart and the new aorta.
Cardiopulmonary bypass was terminated after normothermia.
After bleeding was controlled, the tissues were closed.
The patient was discharged after one day of postoperative
intensive care and 12 days of follow up. During hospitalisation,
antihypertensive and prophylactic antibiotic therapies were
administered. Lifelong antihypertensive treatment was
recommended. No problem was determined at the first month’s
postoperative follow up. After six months, it was observed that
the false lumen was closed on CT angiography.
Discussion
A dissection of the ascending aorta is only rarely circumferential.
Complete circular dissection of the aorta was reported for
the first time by Bostroem in 1887.
1
Hufnagel named this
complication intimo–intimal intussusception.
2
Intussusception
of the internal cylinder in the external aortic cylinder during
circumferential dissection may induce obstruction of the aortic
lumen or obstruction of the ostia of the supra-aortic vessels.
3
Typical features of intimo–intimal intussusception are acute
onset of chest or back pain. Goldberg
et al
. reported that when
A B C
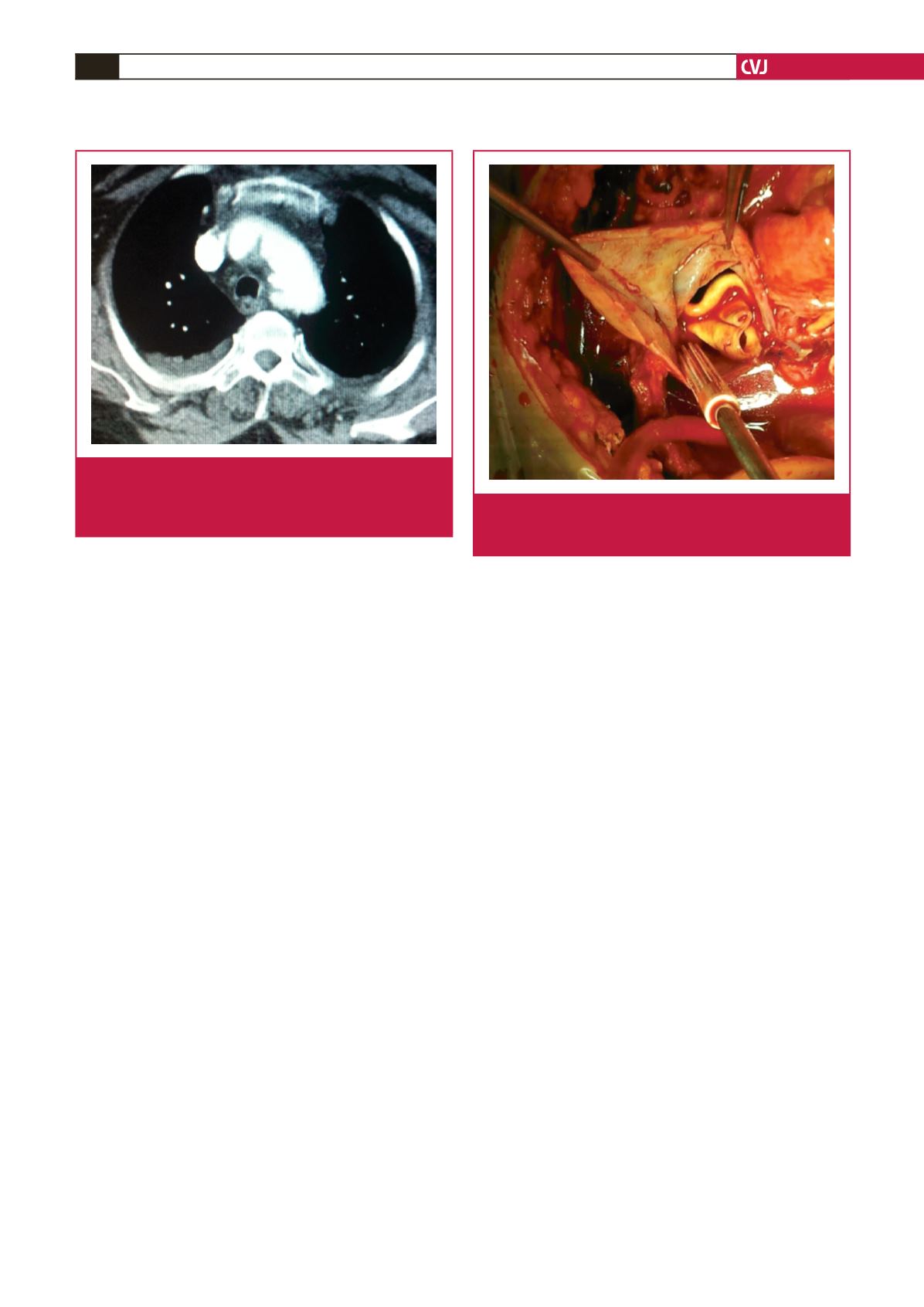
Fig. 1.
Post-contrast axial computed tomography scan demon-
strates intussuscepted dissection flap (A) in aortic arch
with very narrow residual true lumen (C) and a larger
false lumen (B).
Fig. 2.
Photograph during surgery shows total circumferential
intimal tear with intimo–intimal intussusception of the
internal channel into the arch.

















