
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
AFRICA
339
The decision to replace the ascending aorta was based on the
aortic diameter. Patients with an ascending aortic diameter of
more than 45 mm mostly underwent concomitant RAA. In our
study, 80 of 99 patients underwent multiple operations. Nineteen
patients underwent RAA only, 36 underwent AVR and RAA, 25
underwent coronary artery bypass grafting (CABG) and RAA,
11 underwent a Bentall procedure, and eight patients underwent
AVR, CABG and RAA.
AVR + RAA was performed in patients who had aortic valve
stenosis or aortic valve regurgitance and a dilated ascending
aorta with normal aortic sinuses. CABG + RAA was performed
in patients who had coronary artery disease (CAD; coronary
artery stenosis ≥ 70%). The Bentall procedure was performed
in patients who had aortic root aneurysm. If the ascending
aorta was dilated and the aortic root was normal, we replaced
the aortic valve and the supracoronary ascending aorta. If the
non-coronary sinus of valsalva was dilated, we replaced only
the non-coronary sinus by tailoring the supracoronary graft to
extend down to the aortic annulus, but the left and right sinuses
and the coronary arteries were left intact. For patients with
an aortic root abnormality and a dilated ascending aorta, the
Bentall procedure is appropriate.
All surgeries were performed via a median sternotomy
incision. Cardiopulmonary bypass (CPB) was established via
right axillary cannulation and a single venous cannula, and
antegrade and retrograde blood cardioplegia was performed. All
ascending replacements were performed under deep hypothermic
circulatory arrest with a nasopharyngeal temperature of 18
±
1°C. Antegrade cerebral perfusion was used in all patients.
Replacement of the ascending aorta was performed using a
woven Dacron prosthetic graft (AlboGraft LeMaitre Vascular).
If concomitant surgical procedures were required, distal
coronary anastomosis and concomitant surgical procedures
were performed before the replacement of the ascending aorta.
The proximal anastomosis was performed during aortic cross-
clamping and the distal anostomosis was performed under deeep
hypothermic circulatory arrest. After appropriate blood pressure
and cardiovascular stability were ensured, CPB was ended.
Patients were taken to the intensive care unit (ICU) during the
postoperative period.
Statistical analysis
Statistical analysis was performed using SPSS 17.0 for Windows
software (SPSS Inc, Chicago, IL, USA). Data are presented as the
mean
±
standard deviation for the numerical variables (e.g. age,
diameter of ascending aorta) or as the number and percentage
of cases for categorical variables (e.g. mortality, COPD, DM).
Univariate logistic regression analysis was performed to
assess the main factors associated with mortality. Variables in
univariate analysis that were associated with mortality [
p
<
0.20
in the likelihood ratio test (−2LL)] were selected for multivariate
logistic regression analyses.
All identified individual variables were analysed using a
manual backward elimination procedure, starting with a full
multivariate logistic regression model. Variables were kept in
the model if the −2LL ratio test of the model with and without
the variable was significant (
p
<
0.05). The odds ratios (OR) are
presented with 95% confidence intervals (95% CI). The final
individual model was tested using the Hosmer–Lemeshow test
for goodness-of-fit.
Results
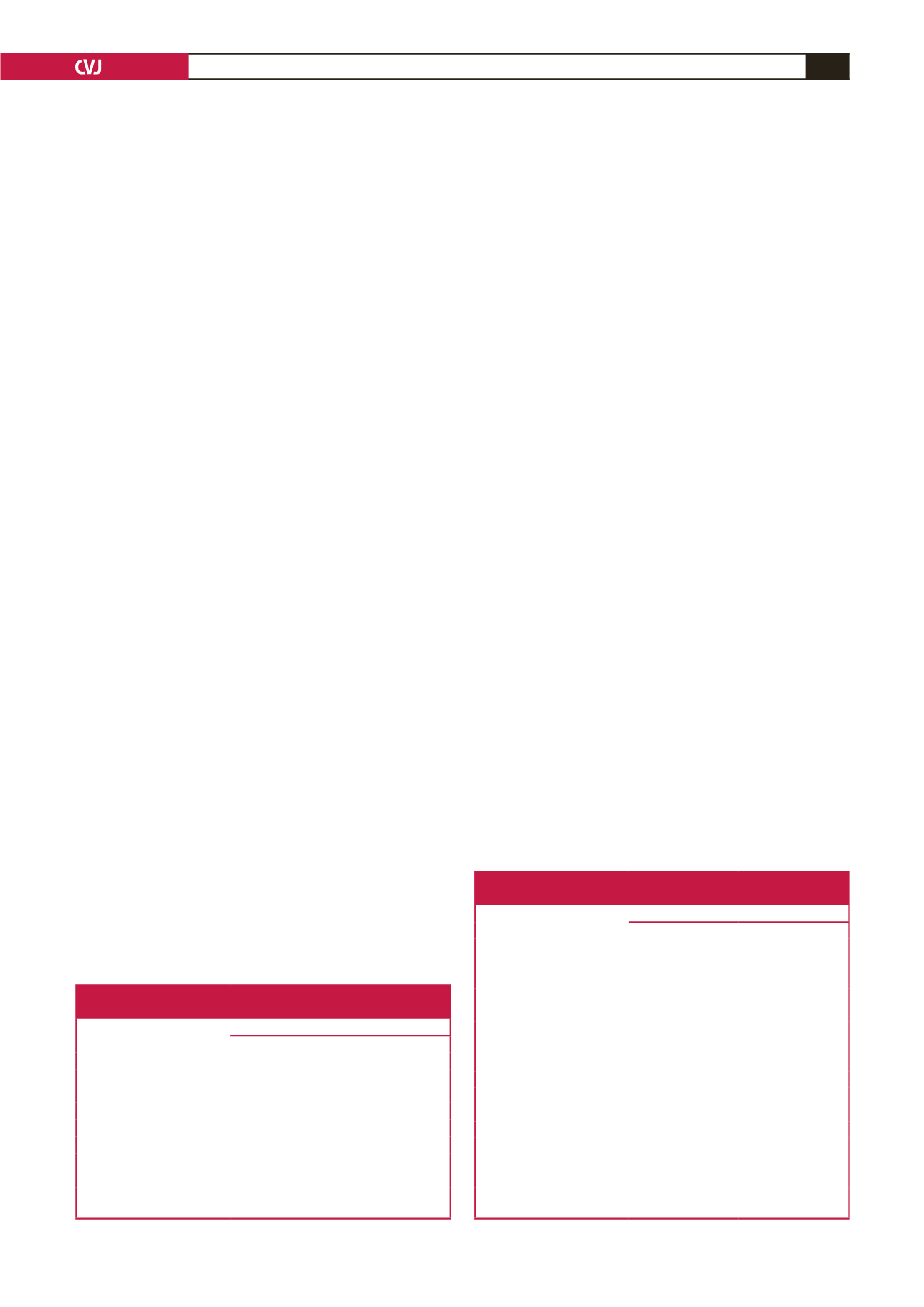
In the patients who died, age, ascending aortic diameter, cross-
clamp time, CPB time, total circulatory arrest time and ICU
stay were longer, bleeding was greater and EF was lower than
the patients who survived (Table 1). The extubation time was
17.2
±
6.13 hours and patients were discharged after 7.30
±
2.41
days. Patients who died had COPD (20%), PAD (20%) and DM
(24%), and required inotrope use (24.6%) and IABP support
(60%) ( Table 2).
Table 3 shows descriptive statistics for patients who
underwent RAA alone and additional surgery. Patients who
underwent AVR + CABG were older (71.3
±
12.74 years) than
those in the other groups. The ascending aortic diameter was
larger in patients who underwent RAA alone (56.2
±
4.03 mm)
compared to the other groups. CPB time and extubation time
in patients who underwent the Bentall procedure (229.5
±
82.79
minutes, 15.6
±
11.36 hours, respectively) were longer and there
was more bleeding (716.7
±
557.9 ml) compared to the other
patients.
Table 4 shows that mortality was 5.3% in patients who
underwent RAA alone, 11.1% in patients who underwent AVR,
Table 1. Descriptive statistics (mean
±
standard deviation)
of the examined variables for mortality
Variables
Mortality
No
Yes
Age (year)
64.3
±
8.46
70.6
±
9.98
Aortic diameter (mm)
52.4
±
5.31
51.8
±
6.79
EF (%)
55.8
±
9.75
47.6
±
11.62
Cross-clamping time (min)
99.3
±
41.16
139.1
±
61.26
CPB time (min)
165.3
±
59.83
193.8
±
65.32
TCA time (min)
25.6
±
7.34
29.2
±
7.05
ICU stay (days)
2.65
±
1.31
10.0
±
14.03
Bleeding (ml)
501.8
±
344.57
725.0
±
381.09
CBP: cardiopulmonary bypass, EF: ejection fraction, ICU: intensive care unit ,
TCA: total circulatuar arrest.
Table 2. Frequencies and percentages [
n
(%)]
of the examined variables for mortality
Variables
Mortality
No
Yes
COPD
No
76 (85.4)
13 (14.6)
Yes
8 (80.0)
2 (20.0)
PAD
No
80 (85.1)
14 (14.9)
Yes
4 (80.0)
1 (20.0)
DM
No
65 (87.8)
9 (12.2)
Yes
19 (76.0)
6 (24.0)
Inotrope use
No
41 (97.6)
1 (2.4)
Yes
43 (75.4)
14 (24.6)
IABP
No
80 (89.9)
9 (10.1)
Yes
4 (40.0)
6 (60.0)
COPD: chronic obstructive pulmonary disease, DM: diabetes mellitus, PAD:
peripheral arterial disease, IABP: intra-aortic balloon pump.

















