
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 1, January/February 2018
28
AFRICA
Descriptive statistics in the form of means and standard
deviations in the case of continuous data, and frequencies and
percentages in the case of categorical data were calculated. A
p
-value of
<
0.05 was considered significant. Ethical approval
for the study was obtained from the University of Pretoria Ethics
Committee (No. 125/2013).
Results
There were 6 536 deliveries at our hospital during the recruitment
phase of the study (1 April 2013 – 30 March 2015). Four
hundred and sixty-three (7.1%) women presented with severe
pre-eclampsia and 106 women were recruited to the study. Ten
women were lost to follow up. Data were therefore recorded for
96 women with severe pre-eclampsia and 45 controls.
Seventy-four (77.1%) women in the study group for whom
data were available fulfilled the World Health Organisation
(WHO) criteria for the classification of a maternal near miss. Of
the 96 women with severe pre-eclampsia, 14 were diagnosed with
chronic hypertension and four with diabetes prior to pregnancy.
At one year, the mean diastolic blood pressure and mean body
mass index was significantly higher among the women who had
pre-sclampsia during pregnancy compared to the normotensive
control group. Table 2 describes the demographic data of the
study population.
Twenty women (20.83%) with pre-eclampsia were diagnosed
with diastolic dysfunction at delivery compared with six (13.3%)
of the controls (
p
=
0.26). Of the 20 women who were diagnosed
with diastolic dysfunction at delivery, 13 (65%) had early-onset
pre-eclampsia, requiring delivery prior to 34 weeks. At one year,
11 (11.46%) women with pre-eclampsia were diagnosed with
diastolic dysfunction compared with three (6.67%) in the control
group (RR
=
1.67;
p
=
0.27).
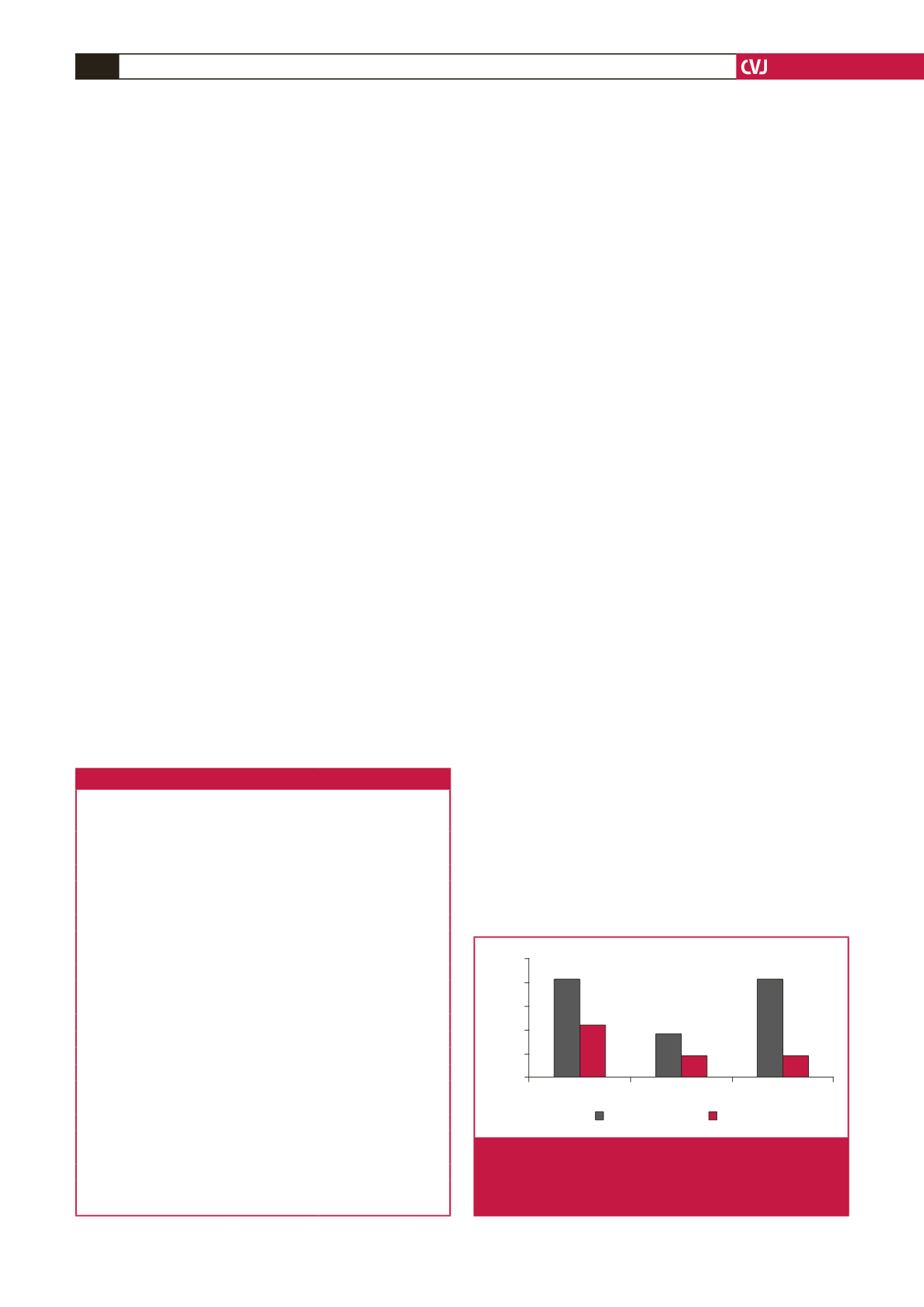
Women with early-onset pre-eclampsia requiring delivery
prior to 34 weeks’ gestation had an increased risk of diastolic
dysfunction at one year post-partum (RR 3.41, 95% CI: 1.11–
10.5,
p
=
0.04) (Fig. 1). Delivery prior to 34 weeks was associated
with an increased risk of diastolic dysfunction even if patients
with chronic hypertension at one year were excluded from
the analysis (
p
=
0.02, 95% CI: 1.43–97.67) There was no
significant association between diastolic dysfunction and chronic
hypertension at one year (RR
=
2.02,
p
=
0.33, 95% CI: 0.57–
7.13). Echocardiographic measurements of diastolic function
after one year are shown in Table 3.
Left ventricular systolic function was normal and similar in
both groups, suggesting preservation of systolic function in both
pre-eclamptics and controls. There was a significant decrease
in lateral e
′
and a significant increase in A velocity between the
pre-eclamptic and control group at one year.
Discussion
Heart failure is a progressive condition, which begins with risk
factors for left ventricular dysfunction and progresses further to
asymptomatic changes in cardiac structure and function, finally
evolving into heart failure.
16
Myocardial remodelling starts
before the onset of symptoms. Diastolic dysfunction precedes
the onset of systolic dysfunction in 50% of cardiac diseases,
which further precedes the onset of heart failure.
5
The American College of Cardiology has highlighted the
importance of identifying asymptomatic cardiac dysfunction for
early intervention and improvement of outcome.
17
The risk for
left ventricular diastolic dysfunction is significantly associated
with higher age, body mass index (BMI), heart rate and systolic
blood pressure.
16
The prevalence of diastolic dysfunction in
a general population aged less than 49 years was found to be
6.8%, and 27.3% for the total population, which included study
subjects older than 70 years.
16
Zanstra
et al
. found that 24% of women with the metabolic
syndrome during pregnancy had diastolic dysfunction at six
months post-partum, compared to 6.3% of women with low-risk
pregnancies.
18
Obesity and diastolic hypertension were strong
correlates to diastolic dysfunction.
The rate of diastolic dysfunction at one year in the two
groups of women with early-onset pre-eclampsia (22.7%) and
low-risk pregnancies (6.7%) in our study were similar to rates
Delivery
1 year
Delivery <34 weeks
25
20
15
10
5
0
Control
Pre-eclamptic
p
=
0.04
p
=
0.27
p
=
0.26
Fig. 1.
Risk of diastolic dysfunction at delivery and at one
year, and at one year for sub-group of women with
early-onset pre-eclampsia requiring delivery prior to
34 weeks.
Table 2. Demographic data of the study population
Characteristics
Pre-eclamptic
group
(
n
=
96)
Control
group
(
n
=
45)
p
-value
Age, years
Mean (SD)
28.9 (6.83)
27.2 (7.14)
0.66
Range
18–46
20–42
Race
African,
n
(%)
86 (89.58)
38 (84.44)
Caucasian,
n
(%)
5 (5.20)
3 (6.67)
Coloured,
n
(%)
4 (4.17)
4 (8.89)
Indian,
n
(%)
1 (1.04)
0 (0)
Obstetric history
Parity mean (range)
1.3 (0–4)
1.6 (0–5)
Timing of delivery
<
34 weeks,
n
(%)
44 (45.83)
0 (0)
34–37 weeks,
n
(%)
25 (26.04)
5 (11.11)
>
37 weeks,
n
(%)
27 (28.13)
40 (88.89)
Medical conditions
Diabetic at 1 year,
n
(%)
6 (6.25)
0 (0)
Hypertensive at 1 year,
n
(%)
52 (54.17)
2 (4.44)
Haemoglobin at 1 year (g/dl)
Mean (SD)
12.02 (1.46)
12.42 (1.13)
0.15
Blood pressure at 1 year (mmHg)
Systolic, mean (SD)
128.01 (14.17)
115.08 (9.89)
0.08
Diastolic, mean (SD)
80.91 (14.47)
72.45 (9.16)
0.001
BMI at 1 year, mean (SD)
30.27 (7.55)
28.04 (3.64)
0.02

















