
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 1, January/February 2018
38
AFRICA
There were 41 patients who were classified as overweight
(BMI
>
25 kg/m
2
,
>
23 kg/m
2
in Indians) and 30 subjects (30%)
were classified as obese (BMI
>
30 kg/m
2
). Increased waist
circumference was found in 44 patients (42 males and two
females). On applying the ethnic-specific harmonised criteria,
48 subjects (48%) were found to have the MetS. The most
prevalent criteria in these subjects were waist circumference,
impaired fasting glucose level and hypertriglyceridaemia (Table
3). Among the subjects without the MetS (
n
=
52), dyslipidaemia
was present in over 40% and there was a high prevalence of
overweight or obesity (65%), a positive family history for CAD
(73%) and smoking (83%).
Hypertension and diabetes mellitus were present in 28 and 26%
of subjects, respectively. There were 20 known (type 1 diabetes
mellitus,
n
=
1) and six newly diagnosed subjects with type 2 diabetes
mellitus. On biochemistry, impaired fasting glucose (
>
5.6 mmol/l)
was present in a further 49 subjects, yielding a 75% prevalence of
dysglycaemia in these subjects (Table 2). The average HbA
1c
level
among subjects with known diabetes was 10.0%, indicating a poor
level of glycaemic control in these subjects.
Seventy-four (74%) subjects had a family history of CAD.
Of these, a history of premature CAD in the immediate family
[a first-degree relative under age 55 (males) or 65 (females)] was
documented in 44 subjects.
Non-conventional risk factors were found in 19 subjects. Of
these, illicit drug use (
n
=
8), retroviral disease (
n
=
2) and alcohol
excess (
n
=
2) were the main factors (Table 4). Of interest, there
was one subject with systemic lupus erythematosus and one with
hypothyroidism. Two patients had co-existing rheumatic valvular
heart disease, but they did not have infective endocarditis or
atrial fibrillation as predisposing factors for coronary embolism.
Four of the five patients who were
≤
25 years at the time of
presentation, had a positive family history of premature CAD
and dyslipidaemia (Table 5). The fifth subject was a 25-year-old
black male patient with a history of smoking and illicit drug use
who had normal epicardial coronary arteries at angiography. It
was suspected that the aetiology in this patient was coronary
spasm related to drug use.
The youngest subject was a 20-year-old Indian male who
presented with an anterior STEMI and was subsequently found
to have non-occlusive disease on angiography with a kinked
distal left anterior descending (LAD) artery. There was no
evidence of hypertrophic obstructive cardiomyopathy (HOCM)
in this case. One Indian patient, aged 25 years, had a long history
of uncontrolled type 1 diabetes mellitus and hypertension. The
remaining two subjects (22-year-old coloured and 24-year-old
Indian males) had three-vessel disease at angiography.
On clinical examination, signs of heart failure (elevated
jugulovenous pressure, lower-limb oedema, pulmonary
crepitations) were identified in 5% of subjects on presentation.
Arrhythmias were identified in eight subjects, four with
tachyarrhythmias [supraventricular tachycardia (
n
=
1),
ventricular tachycardia (
n
=
1), ventricular fibrillation (
n
=
2)]
and four with bradyarrhythmias [first-degree (
n
=
1), second-
degree (
n
=
2) complete heart block (
n
=
1)].
The admission electrocardiogram (ECG) revealed that the
majority of patients (65%) had evidence of anterior ischaemia
or infarction; further classified as anterior (
n
=
9), anterolateral
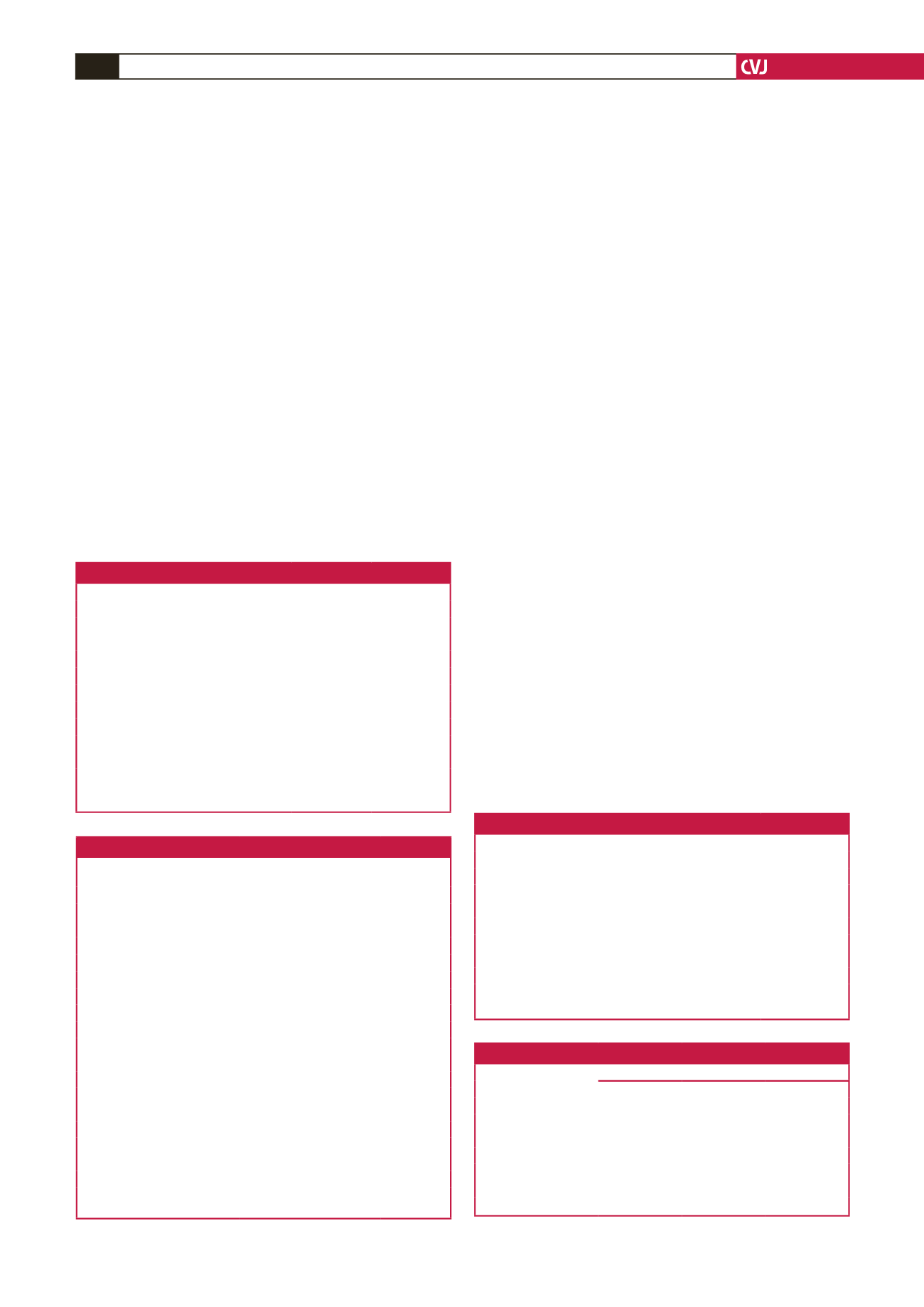
Table 3. Characteristics of subjects with the metabolic syndrome
Characteristics
MetS
(
n
=
48)
No MetS
(
n
=
52)
Total
(
n
=
100)
MetS criteria
WC
>
94 (90)/80
46
14
60
BP
>
130/80
14
9
23
FPG
>
5.6
41
12
53
TG
>
1.7
39
23
62
HDL
<
1.0/1.2
30
21
51
Other factors
BMI
>
25 (23)
47
34
81
Family history
38
38
76
Smoking
40
43
83
Gender
Male
43
47
90
Female
5
5
10
Race
Indian
41
38
79
White
3
8
11
Black
2
5
7
Coloured
2
1
3
WC: waist circumference; BP: blood pressure; FPG: fasting plasma glucose;
TG: triglycerides; HDL: high-density lipoprotein; BMI: body mass index.
Table 4. Non-conventional risk factors
Non-coronary risk factors
Number
Drug use
8
Alcoholism
2
Valvular heart disease
2
HIV
2
SLE
1
Oral contraceptives
1
Hypothyroidism
1
Post-operative
1
Thrombophilia (suspected)
1
SLE: systemic lupus erythematosus.
Table 5. Risk-factor comparison across age groups
Age range, years (
n
)
Risk factors
20–25 (5)
26–30 (18)
31–35 (77)
Smoking,
n
(%)
1 (20)
12 (67)
69 (90)
Hypertension,
n
(%)
1 (20)
7 (39)
20 (26)
Diabetes,
n
(%)
1 (20)
3 (17)
22 (29)
Dyslipidaemia,
n
(%)
4 (80)
16 (89)
60 (78)
Obesity,
n
(%)
0
8 (44)
22 (29)
Family history,
n
(%)
4 (80)
12 (67)
58 (75)
Drugs,
n
(%)
1 (20)
2 (11)
7 (9)
Table 2. Biochemical profile of subjects
Biochemical profile
Number
Percentage
Lipids
TC
>
4.5 mmol/l
62/92
67
TG
>
1.7 mmol/l
58/91
63
HDL-C
<
1 mmol/l (M), 1.2 mmol/l (F)
52/92
56
LDL-C
>
1.8 mmol/l
78/87
90
Glucose
Fasting glucose
>
5.6 mmol/l
49/99
49.5
HbA
1c
>
6.5%
25/97
26
Hb
<
13 g/dl (M), 12 g/dl (F)
10/100
10
Microalbuminuria
24/32
75
TC: total cholesterol; TG: triglycerides; HDL-C: high-density lipoprotein
cholesterol; LDL-C: low-density lipoprotein cholesterol; HbA
1c
glycated haemo-
globin; Hb: haemoglobin.

















