
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 3, May/June 2020
AFRICA
139
subgroups combined, we established that SHD pregnancies
exposed to BBs showed an increase in mean FBW, although
this was not significant. Further analysis of foetal outcomes
between BB-exposed and non-exposed groups within subgroups
revealed significant outcomes for FBW in the cardiomyopathy
and valvular subgroups.
BB usage in the valvular subgroup resulted in a significant
decrease in FBW due, in part, to the predominant use of
atenolol in this subgroup, and given that the use of BB generally
accompanies advanced cardiac disease. Conversely, BB usage in
cardiomyopathy resulted in a non-significant increase in mean
FBW, possibly due to the later mean gestational delivery age. A
second potential causative factor could be the predominant use
of carvedilol in this group.
Most pregnancies within the congenital and valvular
subgroups were prescribed atenolol, which has previously been
shown to decrease FBW.
31
The largest proportion of BB use
occurred within the valvular and cardiomyopathy subgroups
with carvedilol predominantly used as a first-line BB. The
variation in BB prescribing practice can be attributed to patients
having treatment initiated at different sites, which follow different
prescribing protocols. Atenolol is the only BB available in
most primary healthcare facilities in South Africa and is,
therefore, commonly used in patients with valvular heart disease.
Conversely, cardiomyopathy patients are usually referred to a
tertiary hospital for initiation of treatment where carvedilol is
more readily available.
Further dividing the BB-exposed group (
n
=
43) between the
different BBs used, we found an increase in mean FBW trending
toward significance (
p
=
0.094) for pregnancies exposed to
carvedilol (
n
=
16). The difference in FBW found between SHD
pregnancies on atenolol versus those on carvedilol strengthens
the previously mentioned hypothesis that a combined
α
- and
non-selective
β
-receptor blocker (carvedilol) impairs placental
vascular perfusion to a lesser degree than a
β
1-selective blocker
(atenolol).
32
This hypothesis is based on the opposing placental
vascular adrenergic innervation,
β
2-receptor stimulation
causing vasodilation and
α
-receptor stimulation producing
vasoconstriction, which in turn leads to foetal growth retardation.
Although classified as a
β
1-selective blocker, atenolol usage
at increased doses causes
β
2-receptor blockade and therefore
vasoconstriction.
33
Conversely, the vasoconstriction caused
by carvedilol’s non-selective
β
-blockade is opposed by its
concomitant
α
-receptor stimulation and therefore reduces the
possibility of foetal growth retardation.
33
Interestingly, based
on small reports, both drugs were shown to cross the placental
barrier.
34,35
Additionally, higher NYHA functional classes, a clinical
indicator of moderate/severe cardiac impairment, have been
shown to increase adverse foetal outcomes, including SGA.
36
This association, independent of BB usage, may similarly result
from impaired placental perfusion. Atenolol was mostly used
in the valvular subgroup while carvedilol was predominately
used in the cardiomyopathy subgroup. Although underpowered,
our results should encourage re-examination of BB prescribing
Table 3. Impact of maternal SHD severity and HIV on foetal outcome
Variables
NYHA
I/II
(
n
=
148
–
152)
NYHA
III/IV
(
n
=
19
–
21)
p
-value
HIV
negative
(
n
=
134
–
139)
HIV
positive
(
n
=
38)
p
-value
Preterm birth
<
37 weeks 40 (26) 3 (16) 0.409 38 (27) 7 (18) 0.301
Low birth weight
<
2 500 g 46 (31) 6 (29) 0.999 38 (28) 15 (39) 0.169
Apgar score at 1 min
<
7 25 (17) 2 (10) 0.750 19 (14) 8 (21) 0.317
Apgar score at 5 min
<
7 6 (4)
1 (5)
0.590 4 (3)
3 (8)
0.182
Values are
n
(%).
p
-values based on Fisher’s exact tests.
NYHA, New York Heart Association functional class.
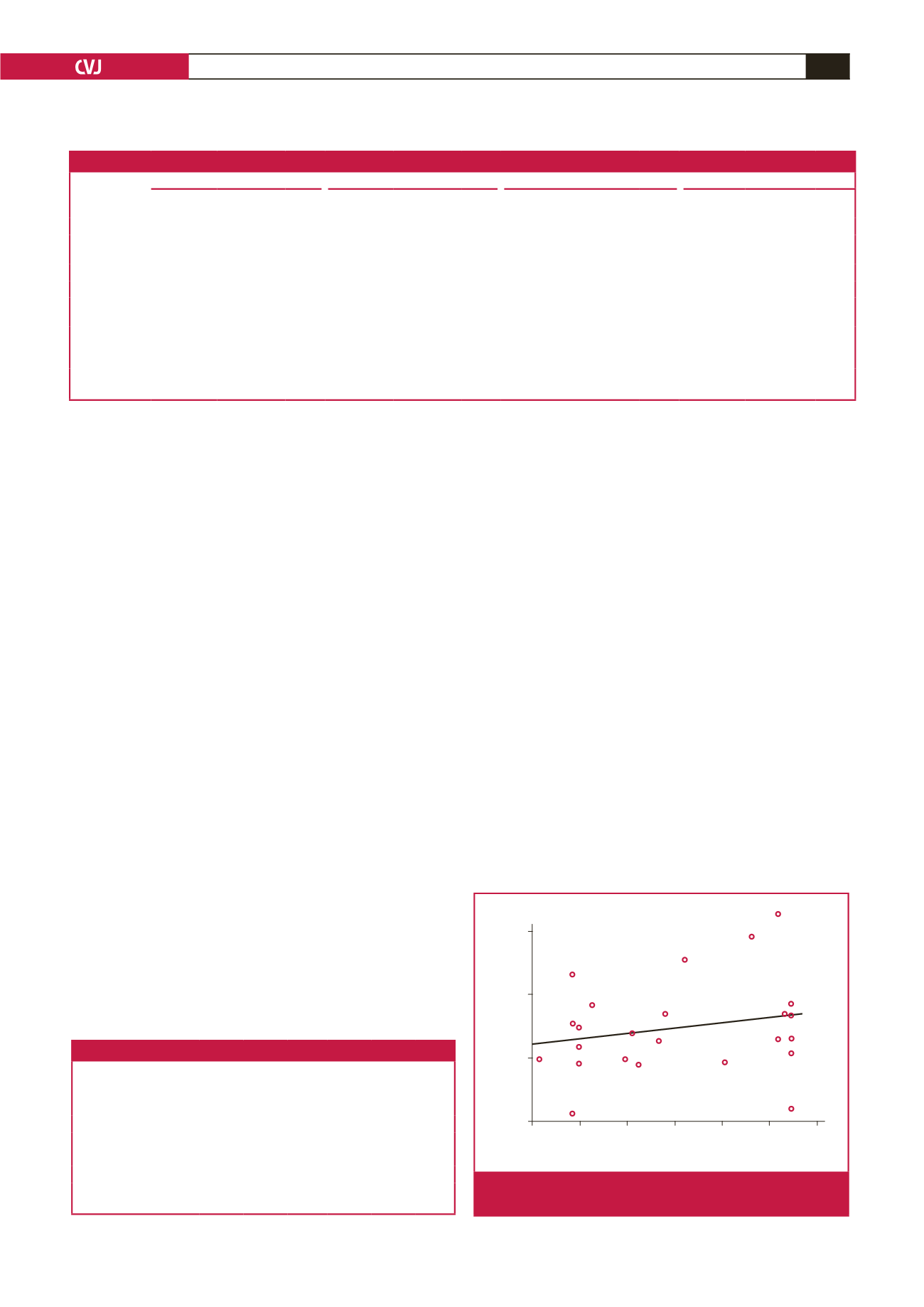
Duration of beta-blocker treatment (days)
Deviation from expected birth weight (%)
0
50
100 150 200 250 300
20
0
–20
–40
Fig. 4.
Scatter plot of duration of BB treatment versus relative
deviation from expected birthweight.
Table 2. Foetal outcomes for structural heart disease pregnancies on BB compared to non-BB usage per subgroup
Congenital
Valvular
Cardiomyopathy
Other
Variables
BB not used
(
n
=
57)
BB used
(
n
=
7)
p
-value
BB not used
(
n
=
45)
BB used
(
n
=
14)
p
-value
BB not used
(
n
=
18)
BB used
(
n
=
18 )
p
-value
BB not used
(
n
=
15)
BB used
(
n
=
4)
p
-value
Apgar score
<
7 10 (17)
1 (14)
1.00
9 (20)
3 (21)
0.938
2 (11)
0 (0)
0.486
2 (13)
0 (0)
0.582
Preterm birth
<
37 weeks
15 (26)
1 (14)
0.669 10 (22)
4 (28)
0.722
5 (28)
5 (28)
1.00
2 (13)
1 (25)
0.530
LBW
<
2 500 g 17 (30)
0 (0)
0.175
4 (9)
6 (43)
0.003
3 (17)
2 (11)
0.630
4 (27)
1 (25)
0.946
SGA
19 (33)
0 (0)
0.094 12 (27)
9 (64)
0.010
3 (17)
2 (11)
0.679
7 (47)
1 (25)
0.435
Gestational age
(weeks)
37.4
±
0.387
[38 (28–41)]
37.6
±
0.782
[38 (33–39)]
0.720 37.6
±
0.293
[38 (33–41)]
37.9
±
0.430
[38 (35–40)]
0.715 36.9
±
0.527
[37.5 (30–41)]
37.4
±
764
[39 (27–40)]
0.152 37.9
±
0.813
[38 (29–41)]
35.8
±
2.29
[37.5 (29–39)]
0.221
Birth weight (g) 2755
±
93.7
[2750 (520–
3930)]
2994
±
103
[3040 (2560–
3440)]
0.319 2906
±
60.9
[2900 (1880–
3640)]
2561
±
121
[2618 (1620–
3322)]
0.009 2774
±
139
[2670 (1370–
3740)]
3225
±
171
[3325 (1725–
4600)]
0.049 2743
±
199
[2863 (820–
3600)]
2594
±
536
[2905 (1085–
3480)]
0.754
Values are mean
±
SD [median (range)] unless otherwise specified.
p
-values based on unpaired
t
-tests with Welch’s correction, Mann–Whitney
U
-tests or Fisher’s exact
tests where appropriate. BB, beta-blocker; SGA, small for gestational age; LBW, low birth weight.



















