CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 4, July/August 2011
AFRICA
199
Her CD
4
T-cell count had declined to 331 cells/
μ
l and HIV viral
load was 60 000 copies/ml (log
10
4.78).
We performed a left pedal artery bypass using a non-reversed,
valve ablated, great saphenous vein and a first toeectomy. She
was discharged 10 days post-operatively with a functioning graft
and a viable left foot. Work-up for ART was begun in hospital,
but she failed to return to clinic to start antiretrovirals.
She presented five months later with an occluded graft,
secondary to sepsis involving the left leg, and an ischaemic left
foot. There was no significant change in her CD
4
T-cell count.
Her HIV viral load had risen to log
10
5.7. Causes of vasculopathy
and pro-coagulant state other than HIV were again ruled out. A
left above-the-knee amputation was performed, with an unevent-
ful post-operative course. She was commenced on antiretroviral
therapy as an inpatient without adverse effects.
Histological review of operative specimens showed no
evidence of atherosclerosis, thrombosis or aneurysms. The small
muscular arteries were thickened (Fig. 1A, B), with reduplication
of the elastic lumina (Fig. 1C) and mucopolysaccharide deposi-
tion in the adventitia (Fig. 1D, E). Some fragmentation of the
tropocollagen was identified (Fig. 1F) and neovascularisation of
the media was noted. There was no obvious vasculitis of the large
vessels, but the adventitia revealed numerous capillaries (not slit-
like) (Fig. 1G, H), and inflammation of the vaso vasorum, with
abundant lymphocytes and plasma cells. These findings have
previously been associated with HIV-associated vasculopathy.
2
Discussion
The clinical entity of HIV-associated vasculopathy encompasses
a spectrum of conditions occurring in HIV-infected persons,
including cardiovascular disease, cerebrovascular disease, arte-
rial aneurysms, peripheral arterial occlusive disease, acute limb
ischaemia, and deep-vein thrombosis. The initial description of
this ‘distinctive arteriopathy’ by Joshi and colleagues in 1987,
emanated from observations on histological specimens from
children with advanced immunosuppression, showing vascu-
lopathy with small and medium-size vessel involvement, intimal
fibrosis, peri-vasculitis, fragmentation of elastic tissue and
medial fibrosis and calcification.
3
HIV-associated vasculopathy tends to affect young patients
at an estimated prevalence of 0.19 to 23%.
4,5
Its epidemiology
remains largely unresolved, as the majority of studies are hospi-
tal-based and therefore not reliably representative of prevalence
and incidence in the general population. Any part of the vascular
tree can be involved, but skin, central nervous system, skel-
etal muscle, lung, kidney and peripheral nerves are commonly
affected.
6
Clinical features are specific to the vascular territory
involved, but typically manifest as either stroke, cardiomyopathy,
pulmonary hypertension, HIV-associated nephropathy or periph-
eral arterial disease in young patients, predominantly under 55
years of age.
7
The aetiology and pathogenesis of HIV-associated vascu-
lopathy is considered to be multi-factorial. Evidence for direct
infection of the endothelium by HIV, and both humoral and
cell-mediated immune injury to the vessels, leading to insidious
or rapid damage to large elastic vessels has been proposed.
2,8,9
HIV-associated vasculopathy involves an exclusively T-cell
lymphocytic infiltrate with oligoclonal expansion of CD
8
+
T
cells that release super antigens, vascular adhesion molecules,
immune complexes, growth factors and cytokines that mediate
inflammation and vascular damage.
10
Others have reported on the preponderance of CD
3
+
CD
8
+
T cells in autopsy specimens of patients with HIV-associated
vasculopathy, and have argued that it is the HIV-related immune
aberration that leads to abundant CD
3
+
CD
8
+
T cells that are large-
ly responsible for mediating HIV-associated vasculitis and vascu-
lopathy through accelerated endothelial cell injury.
11
Vascular
injury caused by a prothrombotic state, malignant atrophic
papulosis, thrombotic micro-angiopathy, systemic vasculitis or
vasculopathy, and arteriolar para-amyloid deposition has also
been identified.
12
Histopathologically, large elastic arteries reveal multiple
aneurysms, occlusions, and areas of stenosis, with no evidence
of atherosclerosis. Microscopically, a leukocytoclastic vasculitis
of the vasa vasora and peri-adventitial vessels has been demon-
strated, with fragmentation of the tropocollagen, as was evident
in our case. Interestingly, there is minimal inflammation of the
media, but with a consistent finding of calcification of the inter-
nal elastic lumina.
2
Chetty was the first to describe the various
histological sub-types of the vasculopathy associated with HIV
infection (Table 1).
2
A commonly utilised classification system
for HIV vasculopathy and other rare HIV-associated vasculitides
has been proposed by Johnson and colleagues (Table 2).
13
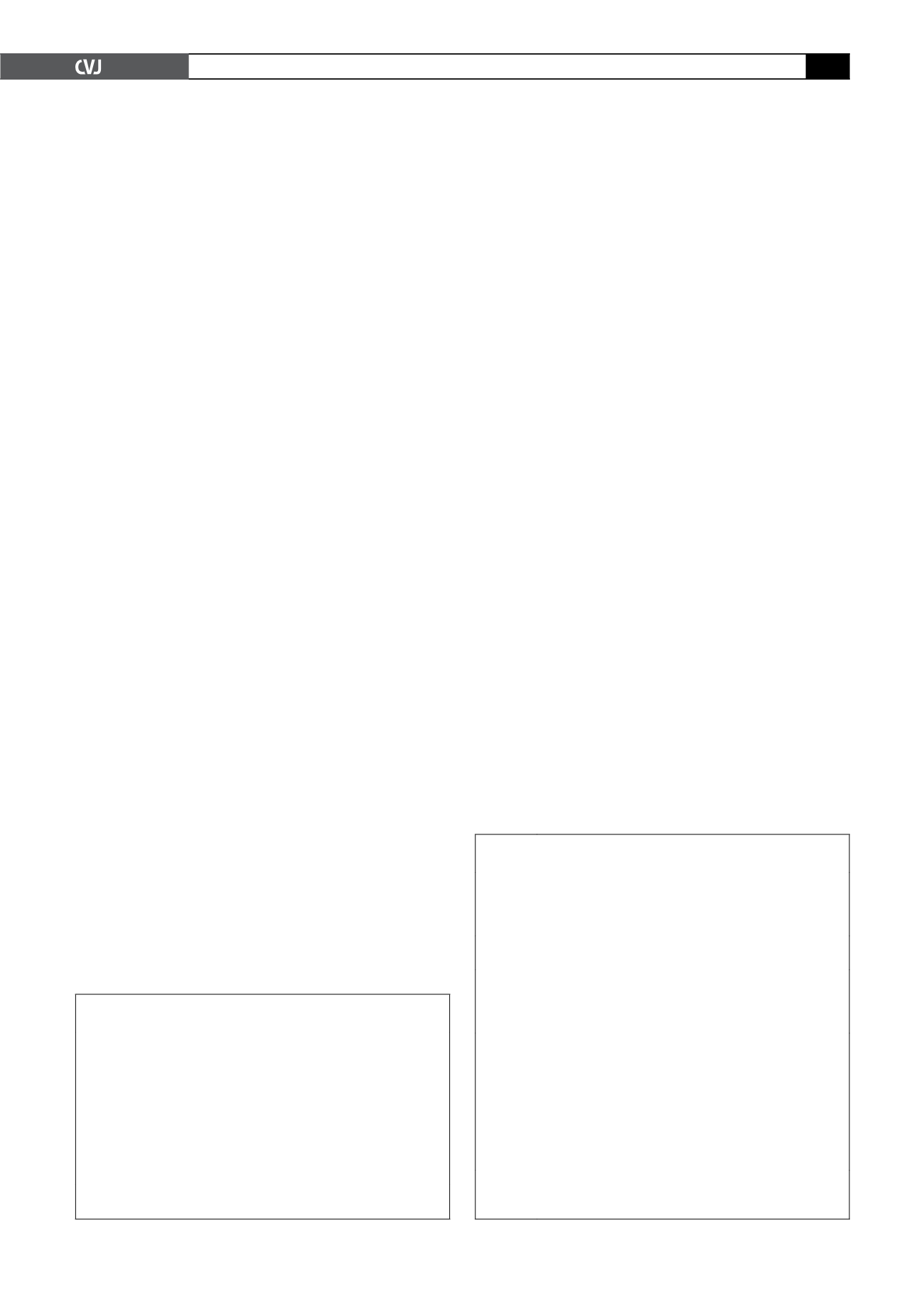
TABLE 1. HISTOLOGICAL SUB-TYPES OF THE
VASCULOPATHYASSOCIATEDWITH HIV
1. Specific infective agents (cytomegalovirus, tuberculosis, syphilis
etc)
2. Polyarteritis nodosa-like necrotising vasculitis
3. Hypersenstivity vasculitis (Henoch-Schonlein purpura, drugs,
cryoglobulins)
4. Angiocentric immunoproliferative vasculitis (benign lymphocytic
angiitis, lymphoma)
5. Granulomatous small-vessel vasculitis/primary CNS angiitis
6. Large-vessel vasculitis/vasculopathy
7. Non-specific vasculitidies
From Chetty R. Vasculitides associated with HIV infection.
J Clin Pathol
2001;
54
: 275–278 (with permission).
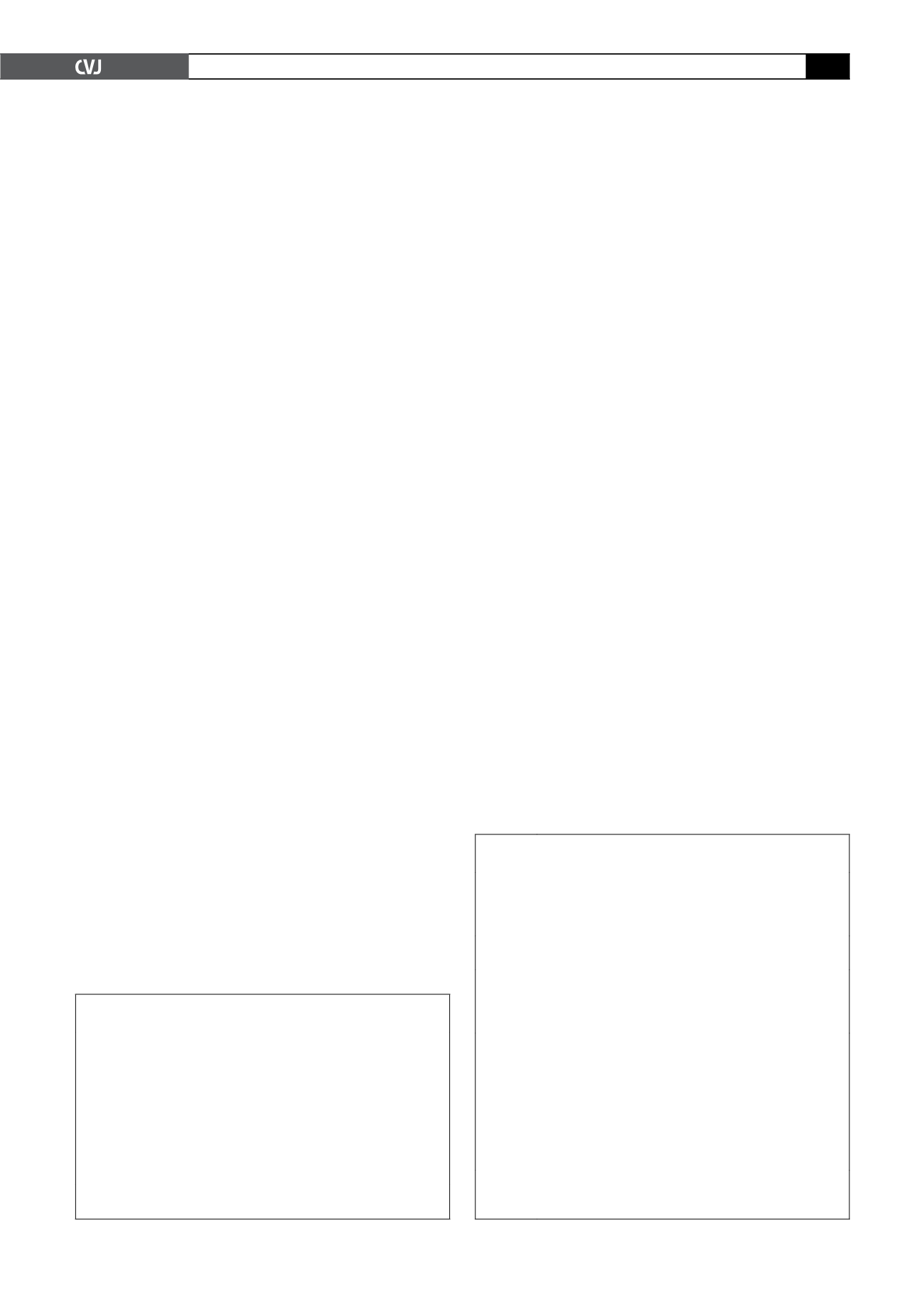
TABLE 2. A CLASSIFICATION SYSTEM FOR
HIV-ASSOCIATEDVASCULITIS/VASCULOPATHY
Group I Vasculitides that are well described in the non-HIV popu-
lation and coincidentally occur in HIV-infected people
(e.g. Takayasu’s arteritis, temporal arteritis, Behcet’s
syndrome, Henoch-Schonlein purpura)
Group II Vasculitides related to adverse effects of drugs (including
antiretroviral drugs and cotrimoxazole)
Group III Vasculitides related to known infectious agents that are
more common in immunosuppression (e.g. cytomegalo-
virus,
Toxoplasma gondii
,
Pneumocystis jirovechii
pneu-
monia, hepatitis B)
Group IV Vasculitides that appear to have an association with
HIV, have unusual clinical presentations that do not fit
into previously described disease entities, where HIV
pathogenesis probably facilitates development, and have
diverse histopathological features that do not represent a
single disease entity (e.g. erythema elevatum diutinum,
microscopic polyangitis, Kawasaki-like syndromes,
primary angiitis of the central nervous system, acute
occlusion syndromes)
Adapted from Johnson RM, Barbarini G, Barbaro G. Kawasaki-like
syndromes and other vasculitic syndromes in HIV-infected patients.
AIDS
2003;
17
(Suppl 1): S7–S82 (with permission).