CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 6, November/December 2011
AFRICA
e5
gradually got worse. Over the next two months he could walk
only about 200 m without pain, which was acute, cramp-like
and recurrent, and mostly resolved spontaneously. On physical
examination, his pulses on the right femoral, popliteal, tibial
and dorsalis pedis arteries were palpated weakly. There were
aphthous ulcers in the oral cavity. The skin pathology test was
positive. Blood pressure measured on the right arm was 110/70
mmHg and his heart rate was 80 beats per minute.
On laboratory examination, his erythrocyte sedimentation
rate was 45 mm/h, white blood cell count was 12 000/mm
3
,
haematocrit was 43%, haemoglobin was 14.4 g/dl, triglycerides
were 100 mg/dl, total cholesterol was 180 mg/dl, high-density
lipoprotein cholesterol was 43 mg/dl, low-density lipoprotein
cholesterol was 118 mg/dl, and very low-density lipoprotein
cholesterol was 20 mg/dl. Serum complements were normal,
there were no anti-nuclear antibodies, and the rheumatoid factor
was negative. His body mass index was 24 kg/m
2
.
Doppler ultrasonography (US) showed 80% stenosis in the
right iliac artery. Since the patient was symptomatic, digital
subtraction angiography was performed. Ninety per cent steno-
sis was detected at the right common iliac artery (Fig. 1), with
a pressure gradient of 32 mmHg, and the patient underwent an
8-mm-diameter stent implantation (express, Boston Scientific,
Natick, MA, USA) into the iliac artery (Fig. 2).
One month later, the symptoms recurred. On Doppler US,
intrastent obstruction was observed. Digital subtraction angio-
graphy was performed and 90% stenosis of the right iliac artery
stent was confirmed (Fig. 3). The gradient was measured across
the stenosis and it was found to be 28 mmHg. Percutaneous
transluminal angioplasty (PTA) was then performed with an
8-mm balloon (Fig. 4). After removal of the 6F vascular sheath,
the artery was manually compressed to assure haemostasis at the
puncture site. The gradient across the stenosis was lowered to 4
mmHg after PTA.
The patient was discharged on day two without any complica-
tions. During the three-year follow up, the patient had no pain
and he could walk regular distances. He had a normal ultra-
sound examination and on intermittent Doppler US controls,
no obstruction was observed in the stent. No femoral aneurysm
appeared.
Discussion
Behçet’s disease has largely been recognised as an unclassified
vasculitis affecting blood vessels of all types and sizes.
5
One kind
of vasculitis is large-artery involvement. Large and small vascu-
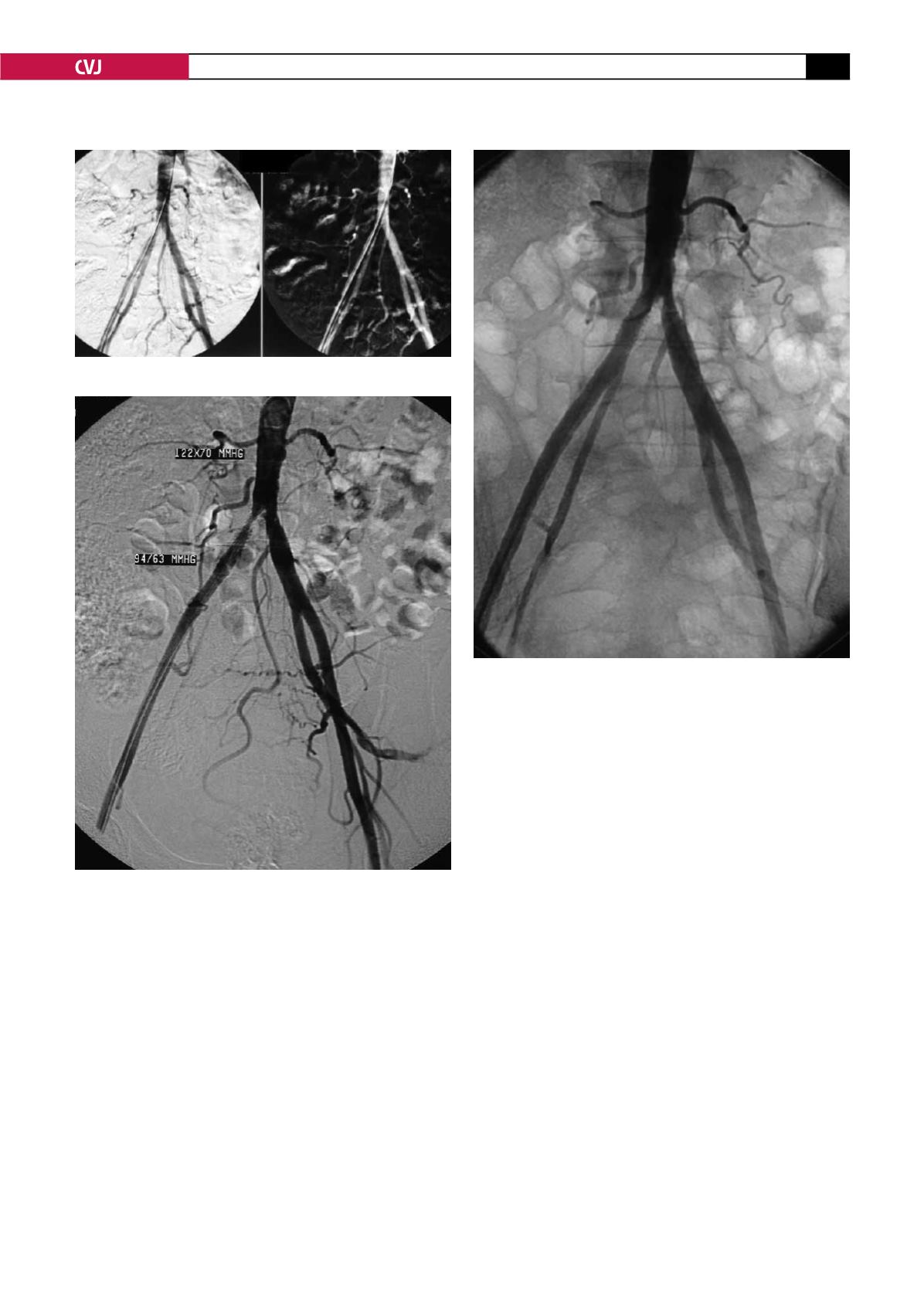
Fig. 2. Application of ipsilateral catheterisation.
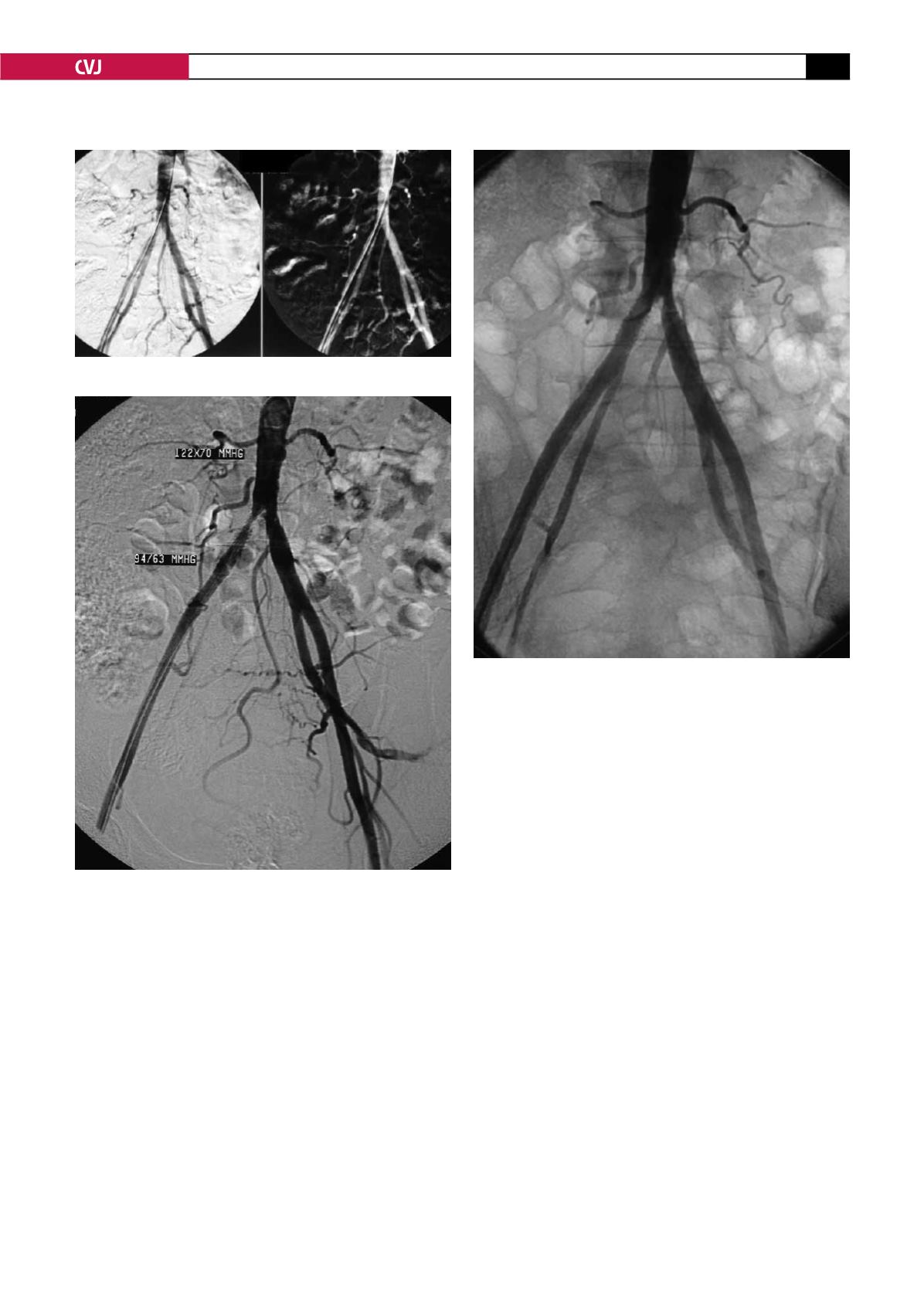
Fig. 4. Application of balloon dilation to the intrastent
stenosis.
Fig. 3. The recurrence of intrastent stenosis after the first
operation.