CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 8, September 2013
AFRICA
e11
cannulation in the right axillary artery, and venous cannula
drainage. After median sternotomy, the ascending aorta was
cross-clamped just proximal to the brachiocephalic artery. The
mean blood pressure of the dorsalis pedis was not satisfactory,
and another cannula was inserted into the femoral artery to
adequately perfuse the lower body.
The patient was slowly cooled to 24°C and aortotomy
was performed. Antegrade direct blood cardioplegia was used
selectively to each coronary ostium to arrest the heart and it was
repeated every 20 minutes. Aortotomy confirmed an intimal
tear situated just 2 cm above the non-coronary sinus with no
extension of the flap beyond the ascending aorta. The aortic
annulus was dilated and the valve was bicuspid, but the valves
were anatomically normal.
A total ascending aortic replacement was performed with
a tube graft of 26 mm, suturing the proximal anastomosis at
the sino-tubular junction and distally to the starting point of
the aortic arch. The brachiocephalic artery was unclamped and
cardiopulmonary bypass was maintained at 4.5 l/min/m
2
to
rewarm the patient. A mean perfusion pressure of 67 mmHg was
maintained, with the lowest perfusion pressure being 55 mmHg
at the initiation of cardiopulmonary bypass.
Intra-operative
transoesophageal
echocardiography
showed neither aortic regurgitation nor any residual valvular
abnormalities. The total cardiopulmonary bypass duration was
130 minutes and total aortic cross-clamp time was 80 minutes.
The patient’s postoperative course was uneventful and he
was discharged on postoperative day 18. Computed tomography
revealed satisfactory repair, and no aortic valve insufficiency
was detected on echocardiograms two weeks and six months
after surgery. Repair of the CoA was scheduled for as soon as
possible.
Discussion
AAD is a life-threatening disease. Complications such as aortic
rupture, cardiac tamponade and acute aortic regurgitation require
immediate surgical intervention. The combination of acute aortic
dissection and CoA is a rare but a significant condition due to
the choice of surgical timing and perfusion methods. Bicuspid
aortic valve is common and occurs in 1–2% of the population.
5
In addition, up to 40% of patients with CoA have an associated
bicuspid aortic valve.
6
As expected, surgery of the AAD combined with CoA
can be more challenging than a simple aneurysm and CoA
repair. Several surgical options are available. Reported treatment
choices include simultaneous repair of an AAD and CoA by
extra-anatomical bypass in a single operation, and sequential
repair of an AAD followed by CoA repair.
As a staged strategy, Sampath and colleagues advocated initial
repair of the CoA to relieve proximal hypertension, so decreasing
the risk of progressive dissection or rupture.
7
This also permits
safe perfusion during repair of the dissection in the second stage
of an operation. On the other hand, replacement of the ascending
aorta can be performed first, followed by repair of the CoA
at a later time.
8-10
Plunkett
et al
. reported a case of a pregnant
patient in which the aneurysm was repaired first using femoral
arterial cannulation, but they had to repair the CoA in the early
postoperative period because of refractory heart failure.
9
Single-stage surgical repair of this combinationwith successful
outcomes has been reported.
11,12
Correction of the CoA first can
solve possible cannulation and perfusion problems. The most
significant difficulties related to a dissected aortic aneurysm are
arterial cannulation and perfusion problems because dissection
impedes cannulation of the ascending and arcus aorta. If
cannulation is performed via a femoral artery, this procedure can
result in perfusion difficulties, especially to the upper extremities
and brain.
Lawson
et al
. reported a case in which they repaired the
CoA first then the AAD.
13
Percutaneous treatment of the CoA
followed by repair of the aortic dissection is another choice of
therapy sequence that may be preferred.
14-15
When a combined single-stage procedure is undertaken, it can
be difficult to provide adequate blood flow on cardiopulmonary
bypass (CPB) to both the upper and lower body. This is because
when the gradient across the coarctation is high, femoral artery
cannulation can deliver adequate blood flow to only the lower
torso and not to the upper torso proximal to the coarctation of the
aorta. Similarly, establishing CPB with cannulation of the distal
arch in patients with coarctation may result in inadequate blood
flow to the lower torso.
When a patient presents with a combination of acute dissection
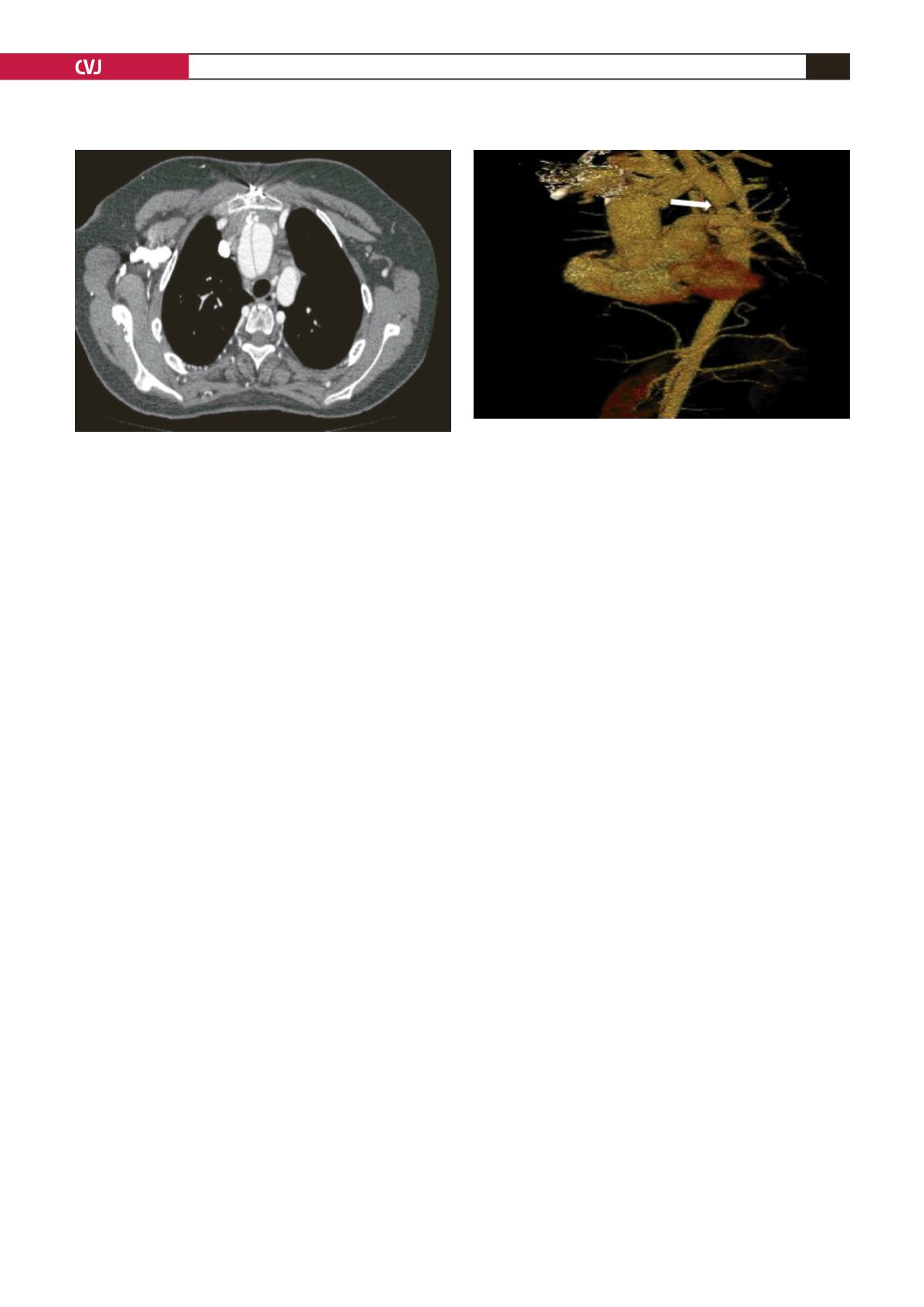
Fig. 2. Computed tomography of the chest demonstrates
the dissection plane with double lumen.
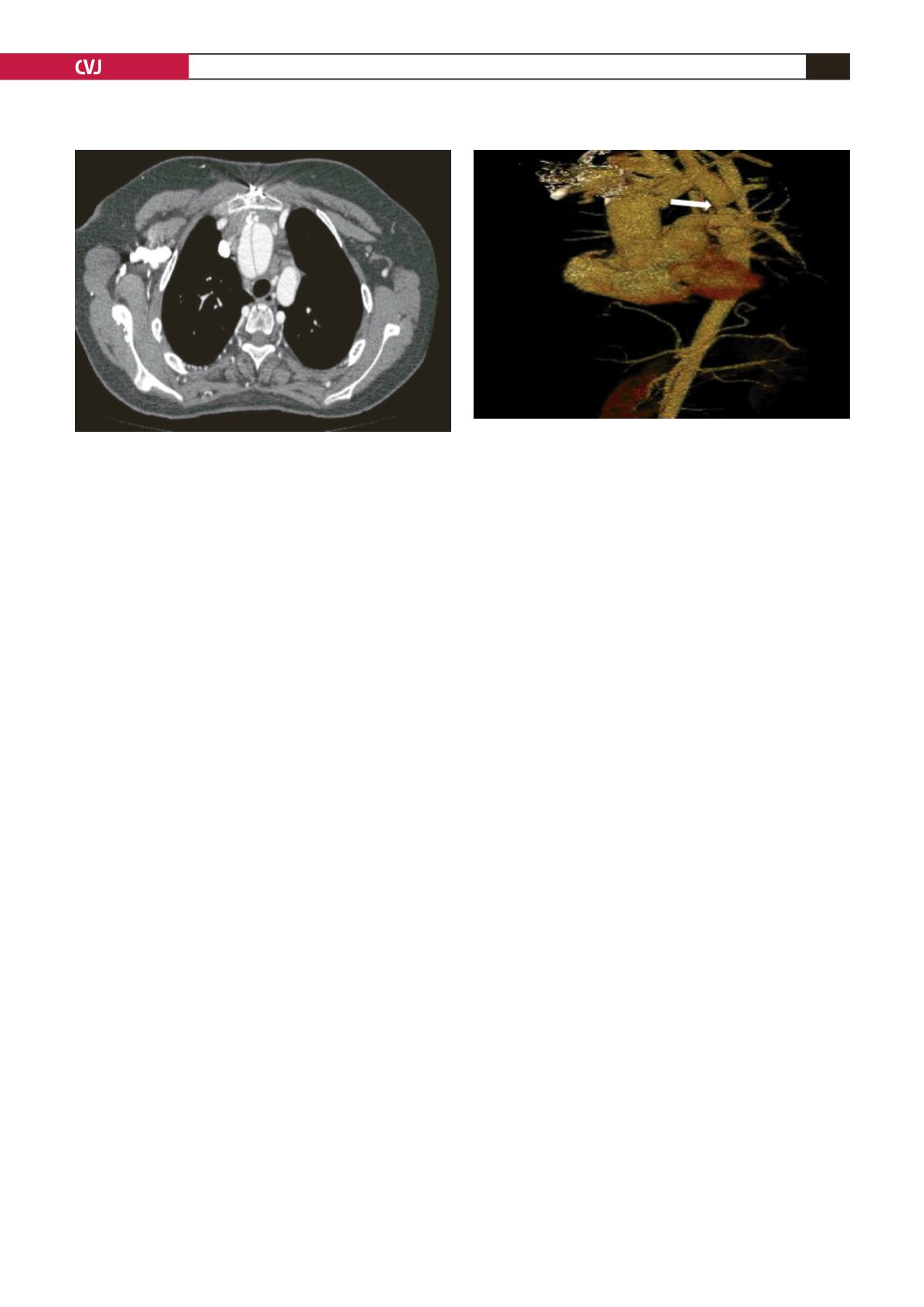
Fig. 3. Computed tomography with three-dimensional
reconstruction reveals coarctation (arrow) at the level of
the aortic isthmus.