CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 8, September 2013
e2
AFRICA
Echocardiography revealed critical mitral stenosis with a
peak gradient of 33 mmHg and mean of 17 mmHg, a dilated
left atrium (55 mm) with severe mitral regurgitation and severe
pulmonary arterial hypertension (mean PAP 66 mmHg). The
mitral valve area was 0.75 cm
2
. The left ventricular ejection
fraction was 0.45.
Cardiac catheterisation revealed two-vessel disease with
stenosis in the left anterior descending artery (LAD) and right
coronary artery (RCA). A pulmonary function test showed
moderate restrictive and obstructive respiratory dysfunction.
Arterial oxygen saturation was 89% when he was receiving 2 l/
min oxygen. On arterial blood gas examination, the partial oxygen
pressure was 64 mmHg, partial carbon dioxide pressurewas 26
mmHg, pH was 7.30 and bicarbonate concentration was 21
mmol/l.
He was accepted for surgery as a high-risk case in view of
the complex nature of the cardiac surgery involving a valve
procedure with coronary bypass grafting (CABG) surgery. A
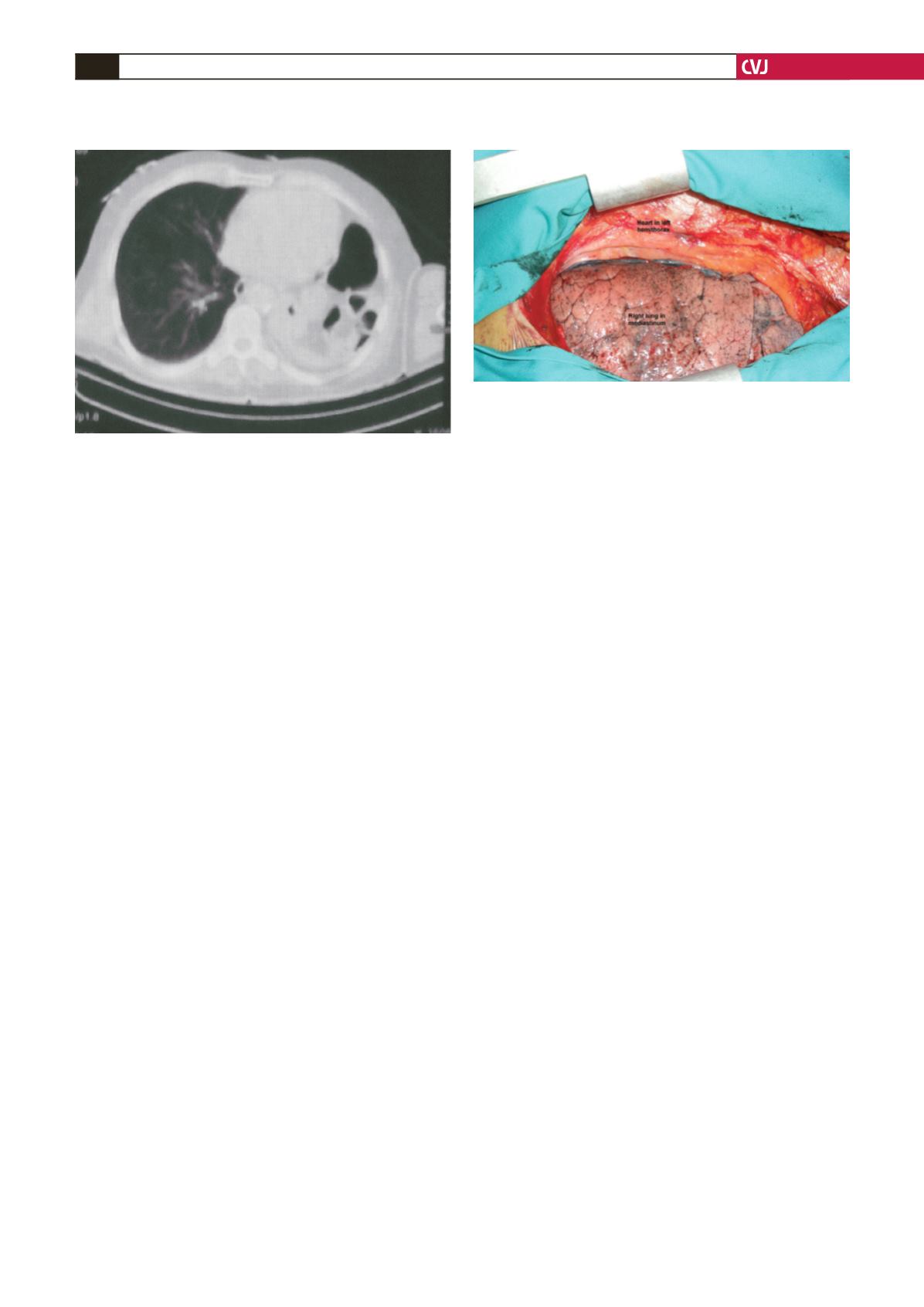
median sternotomy was performed and the right lung was found
to be significantly prolapsing over to the left and the heart was
markedly displaced into the left hemithorax. There were dense
pericardial adhesions and moderate left ventricular hypertrophy.
Stay sutures were required to hold the right lung away and
exposure was quite satisfactory without having to extend the
sternotomy incision laterally. Adequate exposure was provided
for valve and coronary interventions (Fig. 3). A suitable segment
of the saphenous vein was harvested.
Cardiopulmonary bypass (CPB) was initiatedwith the classical
method. Myocardial protection was provided through internal
cold cardioplegic arrest (St Thomas Cardioplegic solution).
Constant blood cardioplegy was given to the retrograde coronary
sinus for maintenance of cardioplegy. Without cross clamping,
a reversed saphenous vein was used to bypass the RCA and
LAD with the beating-heart technique. Then cross clamping was
placed on the ascending aorta.
A left atriotomy was performed and the calcific mitral valve
was excised. The mitral valve replacement was performed
with a number 27 mechanical valve (St Jude Medical). The
cross clamping was removed and proximal anastomoses were
completed to the ascending aorta.
The patient was weaned from CPB without problem. The total
bypass time was 105 min and aortic cross-clamp time was 59
min. Temporary bipolar atrial and ventricular pacing wires were
used and the chest was closed, leaving the pericardium open.
His postoperative course was uneventful. Fluid administration
was restricted during the peri-operative period. He could be
extubated the next morning. Arterial oxygen saturation of the
patient was 90–94% and partial oxygen pressure was 78 mmHg
in the postoperative period. Warfarin sodium (Coumadin 5
mg) was started because of the mechanical valves and a dose
adjustment was done so as to keep the INR value between
2.5 and 3.5. He was discharged from hospital on the ninth
postoperative day. At the six-month follow up he remained in
NewYork Heart Association class I.
Discussion
Performing open-heart operations in patients who have undergone
pneumonectomy presents several problems due to anatomical
and physiological changes.
3,4
This results in a much higher risk
of surgery, especially in the elderly, and requires careful analysis
and management from the pre-operative and intra-operative to
the postoperative periods to have a successful outcome.
Pulmonary dysfunction is a condition that may commonly
be seen after open-heart surgery. Additionally, open-heart
surgery performed on patients who have undergone pulmonary
lobectomy or pneumonectomy may lead to pulmonary problems.
First, a vital capacity reduction related to the previous pulmonary
surgery and pericardial adhesions may be seen. Second,
herniation of the lung to the opposite side may develop due to
mediastinal shift. Besides, anatomical changes in the thoracic
cavity may change the normal relationship and position of the
heart, lungs and great vessels (such as the vena cava). Third,
reduction in pulmonary functions may result in irregularity in
oxygenation due to decreased pulmonary reserve, changes in
ventilation–perfusion rates, pulmonary capillary pressure and
airway pressure. Although these changes are less in patients who
have undergone single lobectomy, they may be more severe in
those who have undergone pneumonectomy.
3-5
When open-heart operations are necessary in patients who
have undergone pneumonectomy, the unavoidable shift of the
mediastinal structures, exposure of the heart, and localisation of
the great vessels and target coronary artery should be carefully
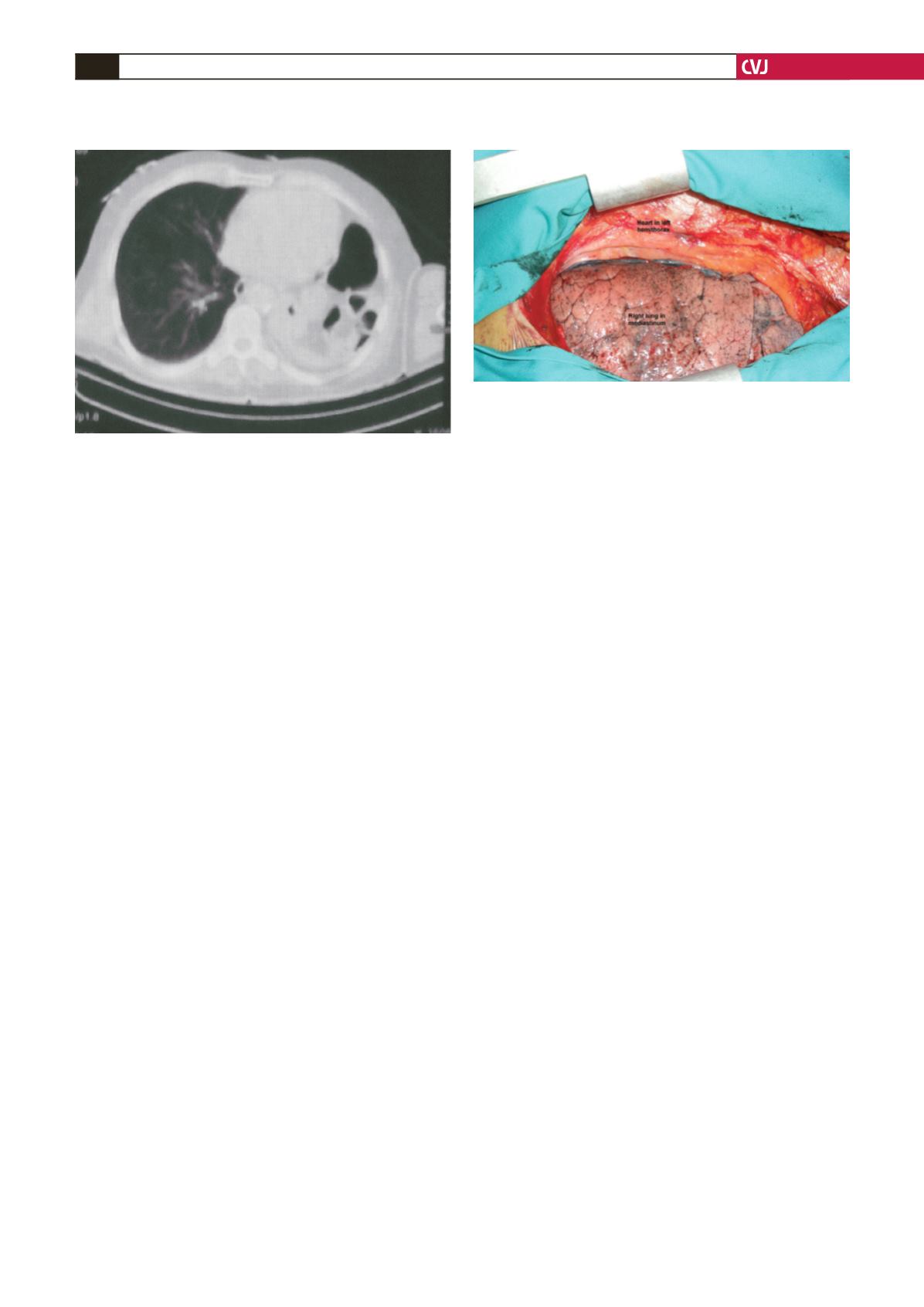
Fig. 2. Pre-operative computed tomography appearance
of a marked shift of the heart and the great vessels into
the left hemithorax with a hyperinflated right lung.
Fig. 3. The right lung is seen to have shifted into the
mediastinal space and the heart into the left hemithorax
on intra-operative imaging.