CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 2, March/April 2014
AFRICA
75
Table 2 shows a comparison of the number of children affected
by a particular risk factor. Some of the children had more than
one risk factor. Among the maternal factors, the most common
risk factors that predisposed to the development of foetal growth
restrictions were maternal infections during pregnancy (
p
<
0.01), and in the symmetrical subgroup, environmental factors
such as smoking (
p
<
0.05) and alcohol consumption by the
pregnant woman (
p
<
0.05).
In oscillometric measurements of blood pressure, there was
a statistically significant difference between the SGA and AGA
groups in DBP (62.92
±
7.32 vs 58.28
±
9.59 mmHg,
p
<
0.05)
but not in SBP (104.73
±
9.66 vs 101.00
±
10.59 mmHg,
p
>
0.05).
Based on ABPM, hypertension was diagnosed in 18% of
the children in the SGA group, while it was not found in any
child in the AGA group (
p
<
0.05). However, abnormal blood
pressure (ABPM meeting the criteria for hypertension or
prehypertension) was diagnosed significantly more often in the
SGA group compared with the AGA group (50 vs 16%,
p
<
0.01). This relationship also occurred in the asymmetrical (53
vs 16%,
p
<
0.01) and symmetrical subgroups (45 vs 16%,
p
<
0.05).
A significantly higher blood pressure load (both systolic
and diastolic) was found in the SGA patients. When comparing
symmetrical and asymmetrical subgroups with the AGA
group, the values of blood pressure load were also statistically
significantly higher (Table 3).
When analysing ABPM measurements more specifically,
we found more significant results. Among children born with
features of asymmetrical IUGR, there were higher mean SBPs
during the daytime (116.03
±
6.71 vs 112.44
±
5.24 mmHg,
p
<
0.05), and MAPs during the daytime (85.17
±
4.95 vs 82.23
±
4.71 mmHg,
p
<
0.05), compared with those of the AGA group.
Patients from the SGA group with a birth weight less than
the 5th percentile were subjected to a separate analysis. In this
group of children, IUGR risk factors also appeared significantly
more often than in the AGA group (environmental factors such
as smoking and alcohol consumption during pregnancy, and
maternal factors) (
p
<
0.05). With oscillometric measurement,
DBP was significantly higher in the subgroup below the 5th
percentile than in the AGA group (63.78
±
7.64 vs 58.28
±
9.59
mmHg,
p
<
0.05) while SBP did not differ significantly.
A significantly higher blood pressure load was also found in
this group compared with children from the AGA group (SBP
load: 25.83
±
21.18 vs 13.72
±
10.86 mmHg,
p
=
0.01; DBP load:
11.22
±
8.20 vs 5.76
±
5.20 mmHg,
p
<
0.01), as well as a higher
mean SBP during the daytime (115.91
±
6.91 vs 112.44
±
5.24
mmHg,
p
<
0.05), higher mean DBP during the 24-hour period
(65.17
±
4.69 vs 62.60
±
3.50 mmHg,
p
<
0.05), and a higher
MAP during the daytime (85.22
±
5.05 vs 82.23
±
4.71 mmHg,
p
<
0.05) and during the 24-hour period (80.57
±
4.81 vs 77.72
±
3.65 mmHg,
p
<
0.05).
The analysis showed a statistically significant negative
correlation between the occurrence of abnormal blood pressure
and birth weight (
r
=
0.29,
p
=
0.01). Nevertheless, the combined
frequency of hypertension together with prehypertension among
the SGA children was compared with the group of children
born with a birth weight
≤
5th percentile and those between the
5th and 10th percentiles. There was no statistically significant
difference in instance of abnormal blood pressure values found
between these two groups.
Echocardiographic examination did not reveal any
abnormalities in cardiac structure and function in either group of
children. In five children from the SGA group and two patients
from the AGA group, left ventricular hypertrophy was found
(according to de Simone or Deveroux). The difference was
not statistically significant. LV mass indices did not correlate
significantly with abnormal blood pressure levels.
The relationship between blood pressure and other
birth parameters, i.e. body length, head circumference and
ponderal index, was also examined. A study was conducted
on the correlation of family history of hypertension and other
cardiovascular diseases with blood pressure values. Factors such
as gender, age of the child at the time of the study, and current
weight, height and BMI were also analysed. None of these
factors correlated significantly with frequency of abnormal
blood pressure values.
Discussion
The results of our study indicate that there were significant
differences in the incidence of abnormal blood pressure values
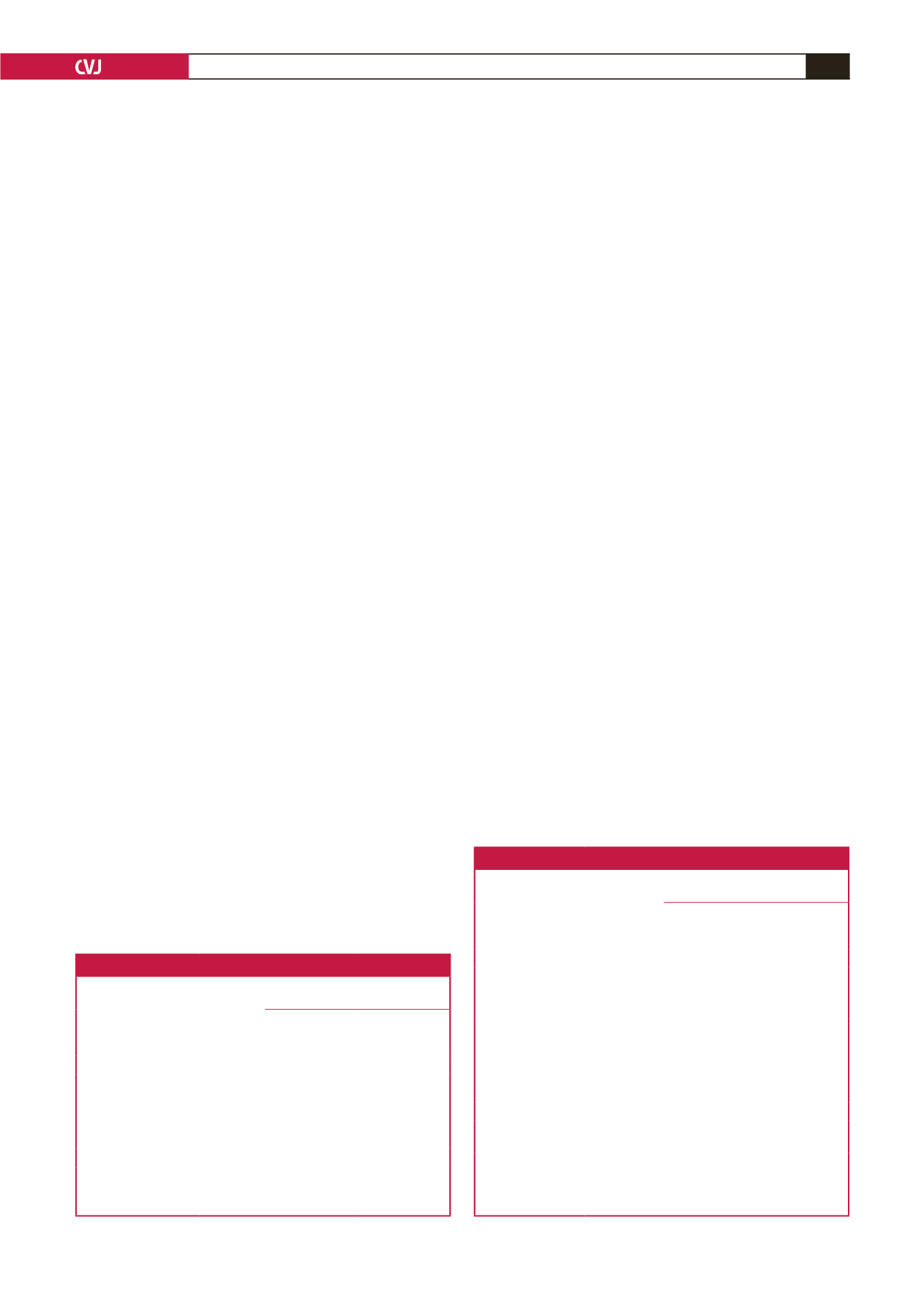
Table 2. The prevalence of risk factors for IUGR
Risk factors
AGA group
(
n
=
25)
SGA group (
p
)
(
n
=
50)
Symmetrical
subgroup (
p
)
(
n
=
20)
Asymmetrical
subgroup (
p
)
(
n
=
30)
Placental factors
0
5 ( NS)
3 (
<
0.05)
2 ( NS)
Maternal factors
4
23 (0.01)
10 (0.01)
13 (
<
0.05)
Environmental factors
5
23 (
<
0.05)
12 (
<
0.01)
11 (NS)
SGA: small for gestational age; AGA: appropriate for gestational age;
p
: statistical significance of the differences in each case was assessed in
relation to the AGA group; NS: not significant.
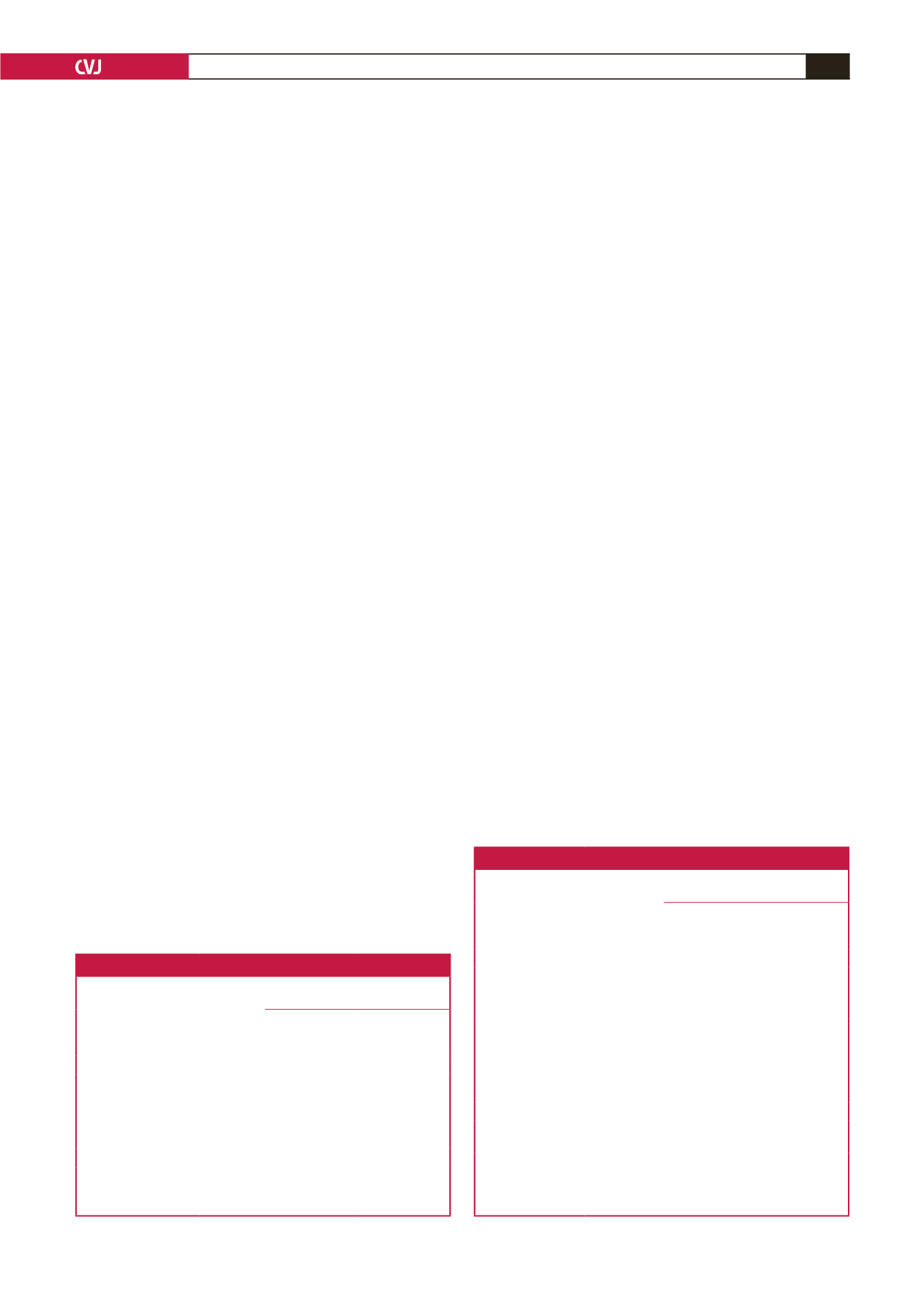
Table 3. Ambulatory blood pressure monitoring parameters.
ABPM parameters
AGA group
(
n
=
25)
SGA group (
p
)
(
n
=
50)
Symmetrical
subgroup (
p
)
(
n
=
20)
Asymmetrical
subgroup (
p
)
(
n
=
30)
SBP load (%)
13.72
±
10.86
24.56
±
20.78 (
<
0.05)
23.45
±
19.10
(
<
0.05)
28.48
±
25.74
(
<
0.05)
DBP load (%)
5.76
±
5.20
10.62
±
9.90 (
<
0.05)
10.05
±
6.53
(
<
0.05)
11.00
±
11.72
(
<
0.05)
Mean SBP (mmHg)
(24-hour period)
107.96
±
5.12
110.86
±
8.57 (NS)
109.65
±
7.03
(NS)
111.67
±
9.48
(
<
0.001)
Mean DBP (mmHg)
(24-hour period)
62.60
±
3.50
64.72
±
5.23 (NS)
64.25
±
4.13
(NS)
65.03
±
5.89
(NS)
SGA: small for gestational age; AGA: appropriate for gestational age;
SBP: systolic blood pressure; DBP: diastolic blood pressure;
p
: statistical
significance of the differences in each case was assessed in relation to the
AGA group; NS: not significant.