
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 5, September/October 2014
208
AFRICA
were deemed fit for surgery. Intervention was scheduled in 38
patients with RHD (86%) [median 19 years (IQR 12–31)] and
in 36 patients (88 %) with CHD [median 4 years (IQR 1–5)].
Eleven patients (13%) presented with co-morbidities or at an
advanced stage and were not considered surgical candidates.
Data concerning major outcomes and surgical follow up are
depicted in Fig. 1.
Twenty-seven patients (14 with RHD and 13 with CHD) were
operated on during the study period, accounting for 36% (27/74)
of patients deemed suitable for surgery. Selection was based
on expected benefit from the surgery, with the most favourable
risk:benefitratio, familial support and patients’ consent. Despite
the low surgical risk, two patients suffering fromDown syndrome
were not considered suitable for heart surgery due to the
expected survival rate in deprived areas. Surgery was performed
after a median waiting time of 10 months (IQR 6–21) in foreign
hospitals funded by NGOs.
Among 14 patients with RHD, 13 (93%) underwent mitral
surgery, both replacement (
n
=
10, 77%) and repair surgery (
n
=
3,
23%) such as annuloplasty, implantation of artificial cordae and
commissurotomy. Combined mitral and aortic valve replacement
was performed in two patients (14%). Tricuspid repair surgery
was performed in four patients (28%).
Among 13 patients with CHD, surgical treatment included
four cases (31%) of VSD closure, two (15%) of AVSD repair,
two (15%) of PDA ligation and one case (8%) of ASD. closure.
Four patients (31%) underwent surgery for complex congenital
defects (two with tetralogy of Fallot, one with aortopulomonary
window, one with persistent truncus arteriosus).
Among 85 patients with HF related to RHD and CHD, 16
(19%) had died by follow up after a median of 38 months (IQR
5–52), and 19 (22%) were lost to follow up (Fig. 1). There were
13 deaths (15%) among patients who did not undergo surgery
despite the presence of clear indications, one peri-operative
death and two late post-operative deaths due to complications
related to mechanical valves (one endocarditis, and one severe
brain haemorrhage).
Nineteen patients (22%) were lost to follow up and were
considered as not operated, given the lack of access to cardiac
surgery in Uganda. Twelve out of the 19 patients lost to follow
up were likely to have died due to to advanced disease at the time
of diagnosis. All patients who had undergone cardiac surgery
experienced improvement in clinical symptoms (22 patients
reverting to NYHA class I; two patients reverting to NYHA
class II).
Discussion
We report here the first prospective hospital-based series of HF
patients in Uganda and show that RHD, a preventable disease,
remains the major cause of HF in a young population. However,
CHD was the leading cause among children, especially those
under 10 years. Other causes were also identified as hypertensive
cardiomyopathy, endomyocardial fibrosis and presumed
ischaemic heart disease. A small fraction of young surgical
candidates had access to treatment through the efforts of NGOs.
We believe our study will add to the knowledge of cardiovascular
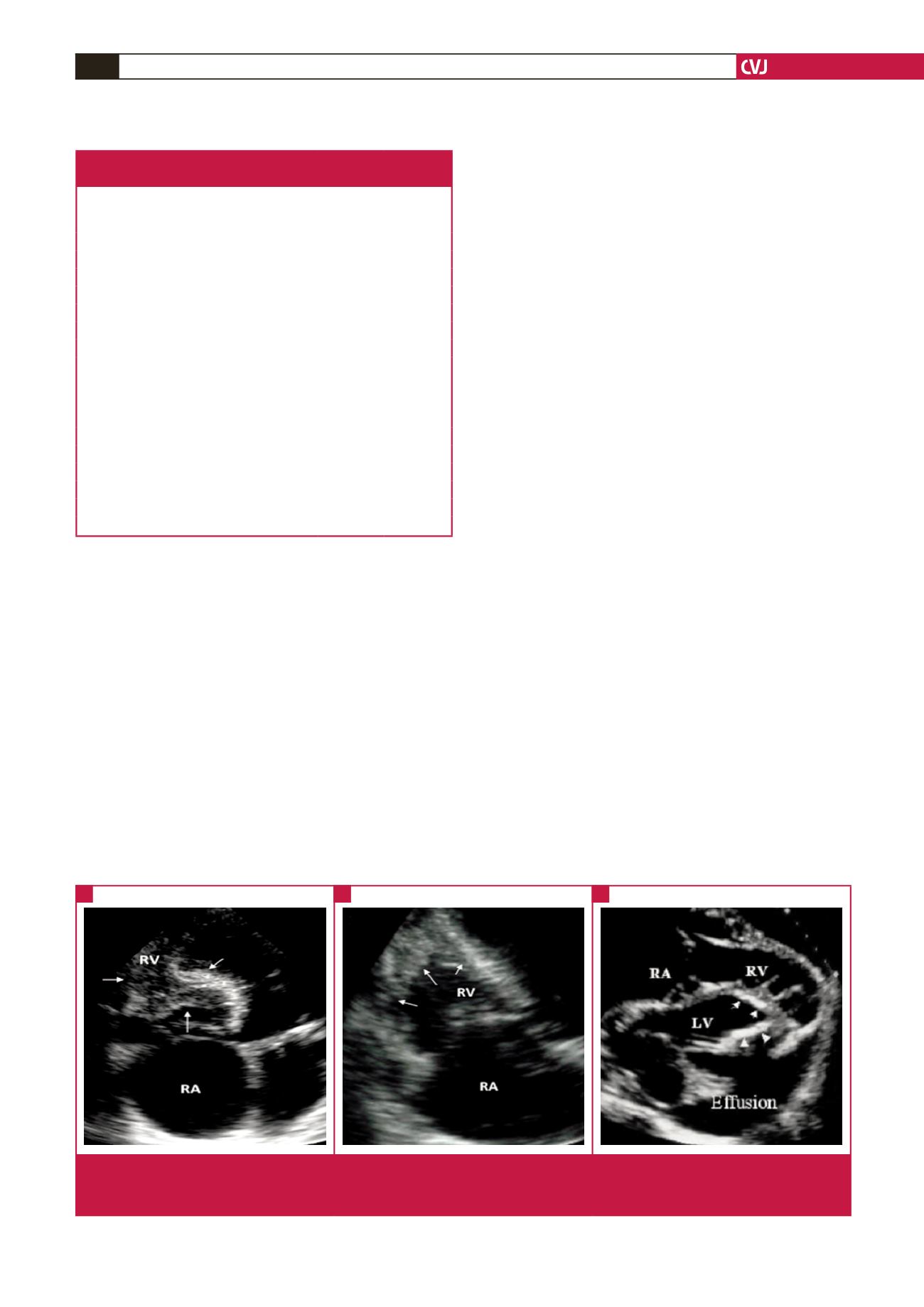
Fig. 4.
Three main patterns of endomyocardial fibrosis (EMF). (A) Fibrotic obliteration of the right ventricular inflow cavity. (B) Limited
fibrotic involvement of the right apex. (C) A rare case of calcified isolated LV EMF. RV = right ventricle, RA = right atrium,
LV = left ventricle.
A
B
C
Table 2. Types of congenital heart defects causing heart failure
in the paediatric and adult populations.
Type of defect,
n
(%)
≤
16-year-
old
n
=
30 (73)
>
16-year-
old
n
=
11 (27)
Total
n
=
41 (29)
Simple defects
19 (63)
8 (73)
27 (66)
Atrial septal defect
3 (10)
3 (27)
6 (15)
Ventricular septal defect (VSD)
7 (23)
0 (0)
7 (17)
Atrio-ventricular septal defect
4 (13)
0 (0)
4 (10)
Congenital mitral cleft
1 (3)
0 (0)
1 (2)
Persistent ductus arteriosus
3 (10)
2 (18)
5 (12)
Congenital aortic regurgitation 0 (0)
1 (9)
1 (2)
RV outflow tract obstruction 1 (3)
2 (18)
3 (7)
Complex defects
11 (37)
3 (27)
14 (34)
Tetralogy of Fallot
4 (13)
1 (9)
5 (12)
VSD + pulmonary stenosis
1 (3)
0
1 (2)
VSD + tricuspid dysplasia
1 (3)
0
1 (2)
Univentricular heart
2 (7)
0
2 (5)
Persistent truncus arteriosus
2 (7)
0
2 (5)
Aorto-pulmonary window
1 (3)
0
1 (2)
Ebstein anomaly
0
2 (18)
2 (5)
Eisenmenger syndrome
0
2 (18)
2 (5)



















