
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
AFRICA
219
predictor of cardiovascular events in hypertensive patients
with diabetes.
22
Hypertension is also a major risk factor for
myocardial infarction and stroke,
12,23,24
and indeed hypertension is
the leading risk factor for mortality worldwide.
5,25-28
Additionally,
hypertension is a major causal factor of end-stage kidney failure,
blindness and non-traumatic amputation in people with diabetes,
where attributable risks are 50, 35 and 35%, respectively.
16
Unfortunately the majority of people with hypertension in
sub-Saharan Africa do not know they have it, and most are not
on treatment. This reflects the low level of knowledge of the
dangers of untreated hypertension in this population.
10
In sub-Saharan Africa there is still a lack of awareness
about the growing problem of NCDs, which, unfortunately, is
often coupled with the absence of a clear policy framework for
prevention and management.
7
Given the long-term decreased
productivity associated with hypertension among diabetics,
identifying and treating a large proportion of patients has the
potential to generate tremendous social and economic benefits
in this region.
5,29-31
In this study we sought to determine the prevalence and
factors associated with hypertension among newly diagnosed
adult diabetic patients in a national referral hospital in Uganda.
These findings are not only necessary, but also contribute to
the diagnosis and management of DM and hypertension in
sub-Saharan Africa.
Methods
This study was carried out in the diabetes out-patient clinic,
the medical endocrine ward and the medical emergency ward
of Mulago National Referral Hospital. It is the only national
referral hospital for Uganda and is the teaching hospital for
Makerere University, with a bed capacity of 1 500. Mulago
Hospital receives referrals from all parts of the country including
from neighbouring countries such as Southern Sudan, the
Democratic Republic of Congo and Rwanda. The study
population is representative of the Ugandan diabetic population.
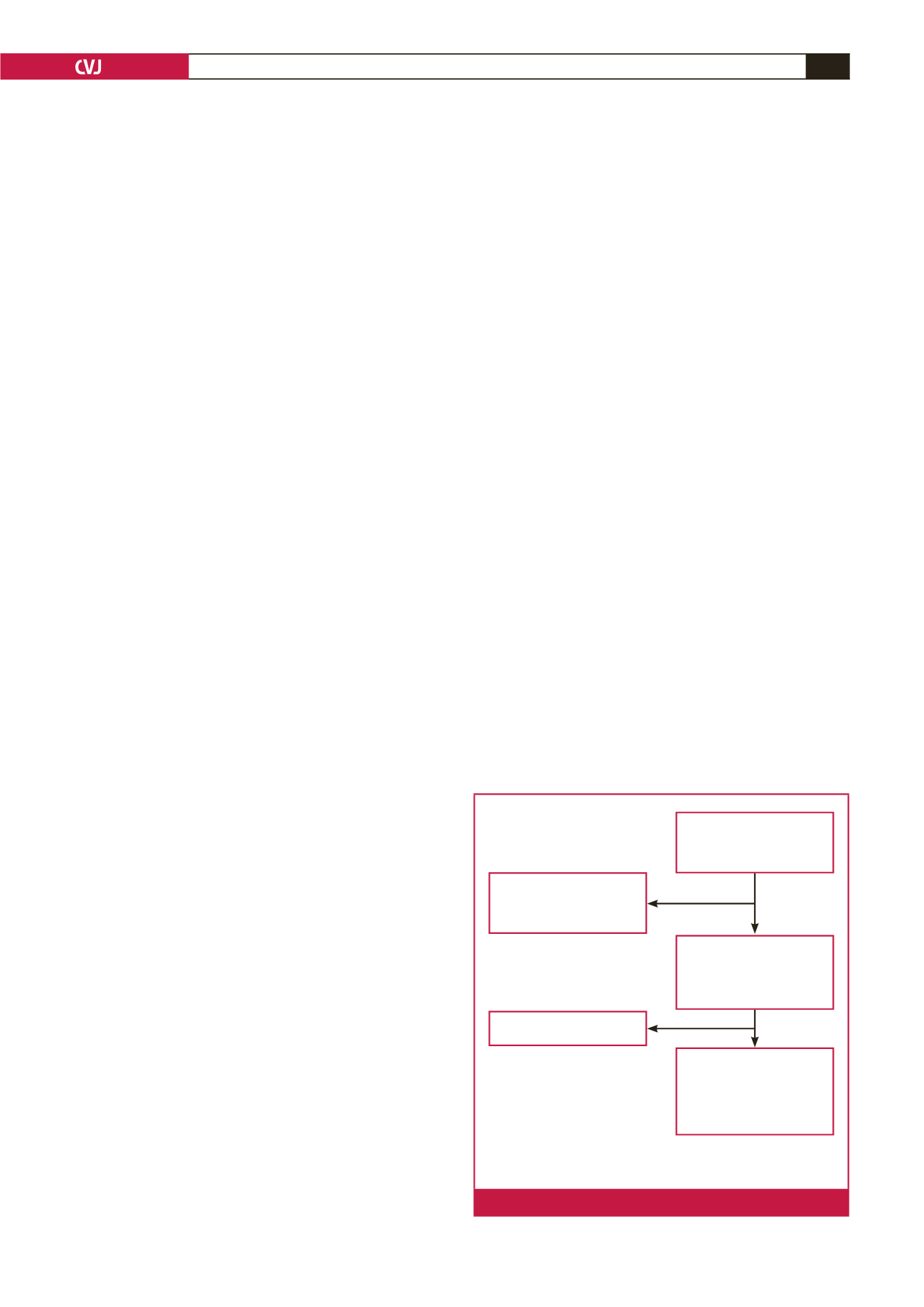
This was a cross-sectional study among 201 newly diagnosed
diabetic patients at Mulago Hospital in Uganda, conducted
between June 2014 and January 2015. All newly diagnosed
diabetic patients aged 18 years and above attending the diabetes
clinic or admitted to the medical wards of Mulago Hospital
during the study period, who met the inclusion criteria and
provided informed consent, were recruited consecutively. We
excluded patients with urinary tract infection in order to avoid
confounding in microalbuminuria, and those who were unable to
provide the necessary information. Fig. 1 illustrates the patient
recruitment flow.
Institutional consent was sought from the Department of
Medicine, Makerere University, Mulago National Referral
Hospital and the School of Medicine research and ethics
committee of Makerere University College of Health Sciences.
All study participants provided written informed consent for
involvement in the study. Enrolment was totally free and
voluntary, and participants were free to withdraw at any time
without any consequences. The patients’ records/information
was anonymised and de-identified prior to analysis.
We took a focused history and performed a specific physical
examination todeterminebiophysicalmeasurements. Information
gathered was entered into a pre-tested questionnaire. We assessed
the following factors: patients’ demographic data, history of
hypertension, age, physical exercise at work and leisure, marital
status, date of diagnosis of DM, drug history, occupation,
education level and last normal menstrual period.
Body mass was measured to the nearest kilogram using a
Secco weighing scale, height was measured in metres using a
non-stretchable tape, and these were used to compute body mass
index (BMI). Waist and hip circumferences were measured and
waist-to-hip ratios were determined for all patients.
Glycated haemoglobin (HbA
1c
) was measured by automated
high-performance liquid chromatography. Other investigations
included urinalysis and microalbuminuria using albumin-to-
creatinine ratio.
Echocardiography parameters were acquired using a
commercially available machine, Phillips HD11XE (Eindhoven,
the Netherlands), with two-dimensional, M-mode and Doppler
capabilities. It was used according to the American Society of
Echocardiography guidelines.
32
Blood pressure was measured using a mercury
sphygmomanometer, according to the American Heart
Association guidelines for the auscultatory method of blood
pressure assessment.
33
The degree of precision of blood pressure
measurement in this study was
±
2 mmHg.
33
Hypertension
was defined as present if subjects were on anti-hypertensive
medication, had a history of hypertension and/or evidence of
hypertension (blood pressure ≥ 140/90 mmHg).
Statistical analysis
Data were double entered in a database developed with Epidata
version 3.1, validated, and inconsistences were cleared. The
data were then exported to Stata 13 for analysis. Continuous
data were summarised using measures of central tendency while
categorical data were summarised as frequencies and percentages
and presented in tables. Prevalence was presented as percentages
Screened 263 newly
diagnosed diabetic patients in
MOPD, Ward 3B Emergency
and Ward 4B Endocrine
Excluded 46:
20: age below 18 years
5: declined to participate
21: too sick to give information
Completed history,
examination and questionnaire
for 218 patients. Performed
urinalysis for microscopy and
ACR. HbA
1c
was determined.
Excluded 16 with
urinary tract infection
Enrolled 201 patients. Cardiac
echo was done for LVH, wall
motion, diastolic and systolic
function by the principle inves-
tigator first and then reviewed
by a cardiologist
MOPD: Mulago out-patient department, ACR: albumin-to-creatinine
ratio, HbA
1c
: glycated haemoglobin, LVH: left ventricular hypertrophy.
Fig. 1.
Patient flow chart.

















