CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 4, July/August 2014
AFRICA
155
Results
Sixty-four patients were entered into the study, with baseline
characteristics as shown in Table 1. All were black South
Africans, mean age 33
±
7 years, and 77% were female. Eleven
patients were excluded on follow up [defaulted on treatment (
n
=
8), pregnant (
n
=
3)].
Mean BMI was 24.8
±
5.4 kg/m
2
and increased to 25.7
±
5.2
kg/m
2
after six months on ART (
p
=
0.39). At baseline, median
CD
4
count was 239 (169–322) cells/mm
3
, and after six months of
ART the CD
4
count increased to 359 (231–411) cells/mm
3
. All
patients had suppressed viral loads.
Thirty patients agreed to participate in the ABP substudy.
Two were excluded at six months due to pregnancy.
There were no significant differences between those who
underwent ABP monitoring and those who did not, according to
age, gender, ethnicity, BMI, CD
4
count, ART status or office BP.
Baseline demographics were similar in the HIV-negative control
group except there were more males in this group compared
with the HIV-positive cohort. However, there was still a greater
percentage of females than males in the control group (Table 1).
At baseline, 13 patients (20%) had an eGFR of 60–89 ml/
min/1.73 m
2
(GFR category G2). No patient had an eGFR
<
60 ml/min/1.73 m
2
(Table 2). Microalbuminuria was present in
three of the 64 patients (4.7%) and only one patient (1.6%) had
macroalbuminuria. At the end of six months, microalbuminuria
persisted in the three patients and developed in two new cases. In
the patient who had initially had macroalbuminuria, it resolved
on follow-up sampling. No patient had a change in eGFR over
the study period.
Mean office SBP increased significantly from 111
±
14 mmHg
at baseline to 116
±
14 mmHg (
p
=
0.05) at six months, but this
was not confirmed by the ABP substudy (Table 2). The mean
day and night ABP values for each group are shown in Table 3.
The mean nocturnal SBP was higher at 110
±
6 mmHg in the
HIV-positive group at baseline compared to 99
±
6 mmHg in the
control group (
p
<
0.0001). There were no significant differences
in age, gender, ethnicity, BMI, CD
4
count, ART status or office
BP between those patients who did and those who did not
undego ABP monitoring.
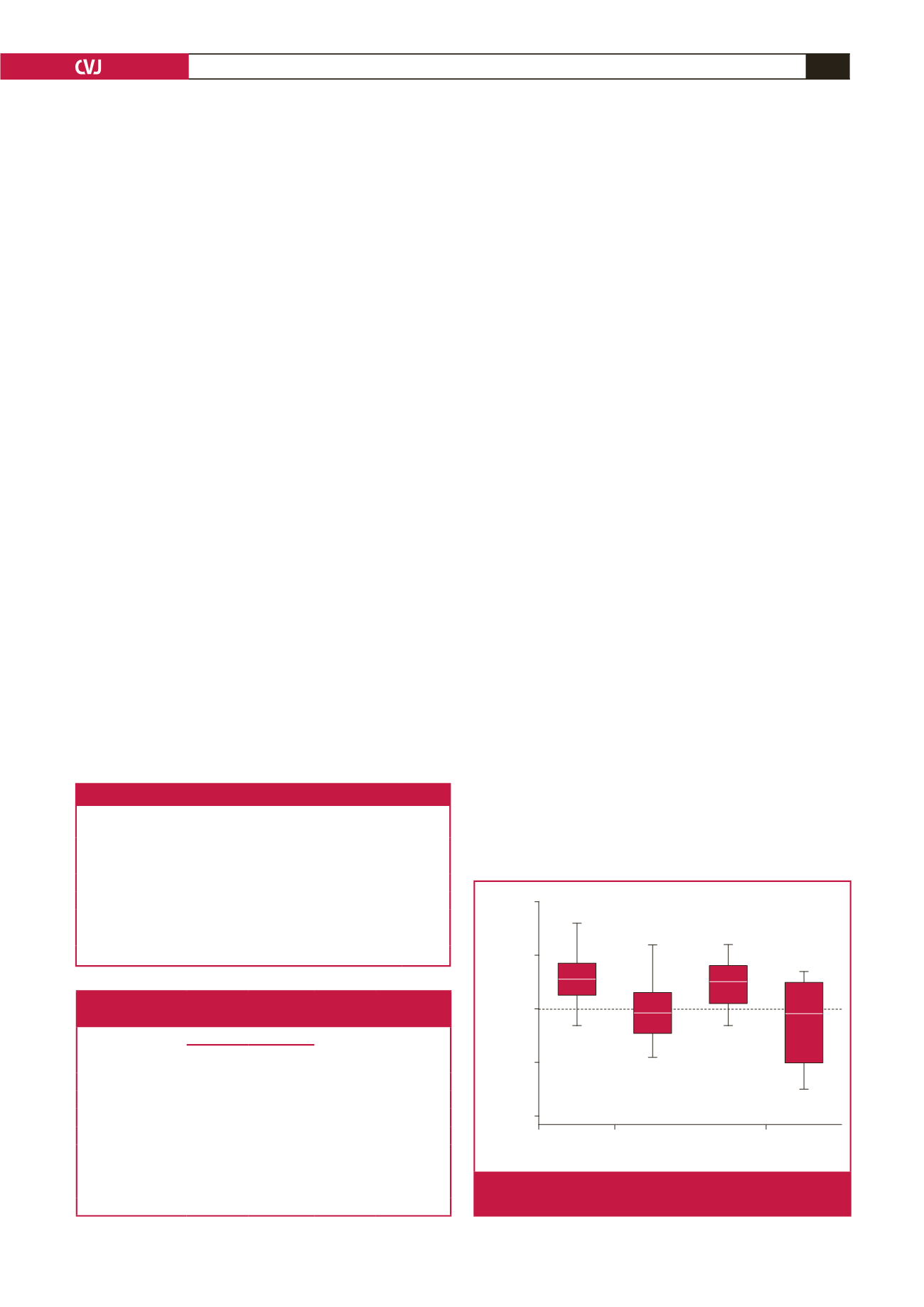
The prevalence of non-dipping in HIV-positive patients (Table
3) did not differ at baseline or after six months on ART. Twenty-
four of 30 subjects (80%) were non-dippers at baseline and 23 of
28 subjects (82%) (odds ratio
=
1.15,
p
=
0.84, 95% CI: 0.31–4.29)
were non-dippers at six months (Fig. 2). In the HIV-negative
control group, nine of 17 (52.9%) were non-dippers; therefore
non-dipping was 3.6 times more likely in HIV-positive patients at
baseline than in controls (
p
=
0.05, 95% CI: 0.96–13.13).
Discussion
This is the first study from Africa, to our knowledge, to have used
ABP monitoring to characterise differences in nocturnal blood
pressure dipping status between HIV-positive and HIV-negative
patients. The study found that: (1) there was a low prevalence
of CKD and microalbuminuria in the healthy HIV-positive
patients; (2) there was a greater prevalence of non-dipping
of nocturnal blood pressure in HIV-positive patients than
HIV-negative controls.
Studies from a high-income country found the estimated
prevalence of CKD in HIV-infected subjects to be 11 to 15.5%.
23,24
Our study found a lower prevalence of microalbuminuria in
HIV-positive patients. In contrast, a study from Johannesburg
reported a prevalence of microalbuminuria of 18.5% in their
cohort of HIV-positive patients.
25
A possible explanation for
this difference is that their patients were significantly more
immunosuppressed (CD
4
<
200 cells/mm
3
), with a mean CD
4
count of 130 cells/mm
3
. They also had a high prevalence of
co-morbid disease, whereas the patients in our study were all
healthy, with a mean CD
4
count of 239–339 cells/mm
3
.
Microalbuminuria is an important finding in HIV as it may
reflect early kidney disease. In a study from KwaZulu-Natal, six
of 25 (24%) patients with an eGFR
>
60 ml/min/1.73 m
2
had
persistent microalbuminuria and HIV-associated nephropathy
(HIVAN) detected on renal biopsy.
26
This is an isolated study.
Table 2. BP and renal parameters at baseline and six months
Baseline
(
n
=
64)
Six months
(
n
=
53)
p
-value
MDRD eGFR (ml/min/1.73 m
2
)
109
±
23 107
±
22 0.66
≥
90,
n
(%)
51 (80)
51 (80)
–
60–89,
n
(%)
13 (20)
13 (20)
–
<
60,
n
(%)
0 (0)
0 (0)
–
Microalbuminuria (mg)
0.9
±
5.0 0.8
±
2.8 0.67
Office systolic BP (mmHg)
111
±
14 116
±
14 0.05
Office diastolic BP (mmHg)
72
±
9
75
±
10 0.69
10
0
–10
–20
–30
Systolic Diastolic Systolic Diastolic
Baseline
6 months
Nocturnal (10 pm to 6 am) dip in blood pressure
Fig. 2.
Dipping status for systolic and diastolic BP at baseline
(n
=
30) and at six months (n
=
28).
Table 3. Mean day and night BP and dipping status in 30
patients with HIV and in 17 control subjects
HIV positive
HIV
negative
Baseline BP
vs controls
(
p
-value)
Baseline Six months
Mean BP (mmHg)
Daytime SBP 114
±
10 116
±
12 114
±
14
1.00
Daytime DBP 75
±
12 72
±
11 73
±
16
0.63
Night-time SBP 110
±
6 111
±
4 99
±
6
<
0.0001
Night-time DBP 65
±
8 67
±
11 60
±
9
0.05
Non-dipper,
n
(%)
24 (80)
23 (82)
9 (52.9)
–
Dipper,
n
(%)
6 (20)
5 (18)
8 (47.1)
0.05
Total
30
28
17
–