CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 4, July/August 2014
162
AFRICA
a major trauma, 46 (4.5%) had hip fractures, 27 (2.7%) had head
injuries while the rest had mixed types of trauma or other forms
of trauma. Orthotrauma and gynaecological conditions were
the commonest causes/reasons for post-admission operations
among the surgical patients with 219 (21.6%) and 169 (16.6%)
undergoing the respective operations. Forty patients (5.7%) had
operations due to cancer.
Sixty-two (6.1%) surgical patients had operations performed
prior to admission, while 437 (43%) had operations performed
within the first two days of admission. A total of 271 (38.5%)
of the surgical patients had emergency surgery performed. Risk
factors for VTE that were present before admission are shown
in Table 3.
Of the 798 patients at risk of VTE prior to admission, 471
(59.0 %) were female; the median age was 54.07 (IQR 39–66)
years. In the surgical population, the most common risk factors
for VTE prior to hospitalisation were obesity, pregnancy, long-
term immobility and chronic pulmonary disease, whereas chronic
heart failure, obesity and chronic pulmonary disease were the
commonest in the medical population (Table 4). VTE risk factors
in patients during hospitalisation are shown in Table 4.
Some patients (surgical and medical) presented with more
than one VTE risk factor, and these are shown in Table 5.
The most common post-admission risk factors to VTE for
both surgical and medical patients were immobilisation with
bathroom privileges, complete immobilisation, and admission to
intensive care unit (Table 6).
Table 7 shows the contra-indications to pharmacological VTE
prophylaxis. Receiving an NSAID on admission and bleeding
on admission were the most common contra-indications to
pharmacological prophylaxis in surgical patients. In medical
patients, significant renal impairment and receiving an NSAID
(including aspirin) on admission were the most common contra-
indications (Table 7). Of the population at risk for VTE, 112
(25.2%) surgical patients and 115 (32.6%) medical patients were
considered to have a high bleeding risk, sufficient to present a
contra-indication to anticoagulant prophylaxis.
Of patients deemed to be at risk for VTE, 411 (51.5%)
received ACCP-recommended types of prophylaxis, of whom
283 (64%) were surgical patients and 128 (36.2%) were medical
patients. Anticoagulants were the most frequently used form of
VTE prophylaxis in the at-risk population; low-molecular weight
heparin was the most commonly prescribed anticoagulant
(Table 8). Mechanical prophylaxis (foot pump and graduated
compression stockings) were used more frequently in surgical
patients than in medical patients.
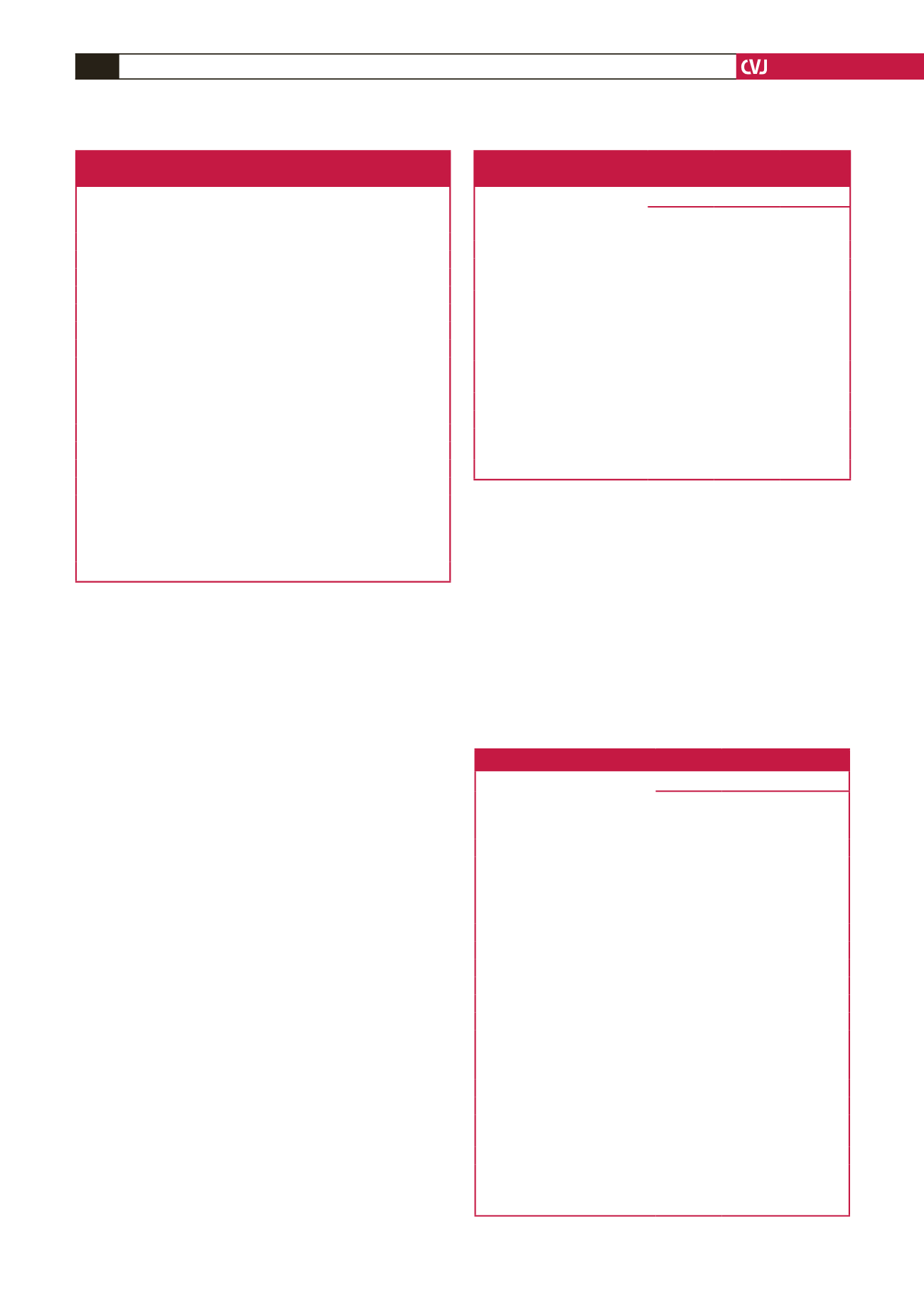
Table 3. Characteristics and reasons for admission
of assessable medical patients
Reason for hospitalisation
Met VTE risk
criteria
(n
=
353) (%)
Did not meet
VTE risk criteria
(n
=
214) (%)
Age, mean
±
SD
63.0
±
12.8
59.0
±
12.2
Gender, M (%)
103 (48.1)
174 (49.3)
F (%)
111 (51.9)
179 (50.7)
Acute heart failure
179 (50.7)
–
Ischaemic stroke
113 (32.0)
–
Haemorrhagic stroke
32 (9.1)
–
Other cardiovascular disease
277 (78.5)
143 (66.8)
Haematological diseases
50 (14.2)
38 (17.7)
Malignancy (active)
42 (11.9)
–
Acute non-infectious respiratory
disease
42 (11.9)
–
Pulmonary infection
136 (38.5)
–
Infection (non-respiratory)
49 (13.9)
86 (40.2)
Haematological or inflammatory
18 (5.1)
23 (10.7)
Neurological disease
21 (5.9)
38 (17.7)
Renal disease
59 (16.7)
67 (31.3)
Endocrine/metabolic disease
100 (28.3)
101 (47.2)
Gastrointestinal/hepatobiliary
disease
46 (13.0)
42 (19.6)
Other medical conditions
37 (10.5)
47 (22.0)
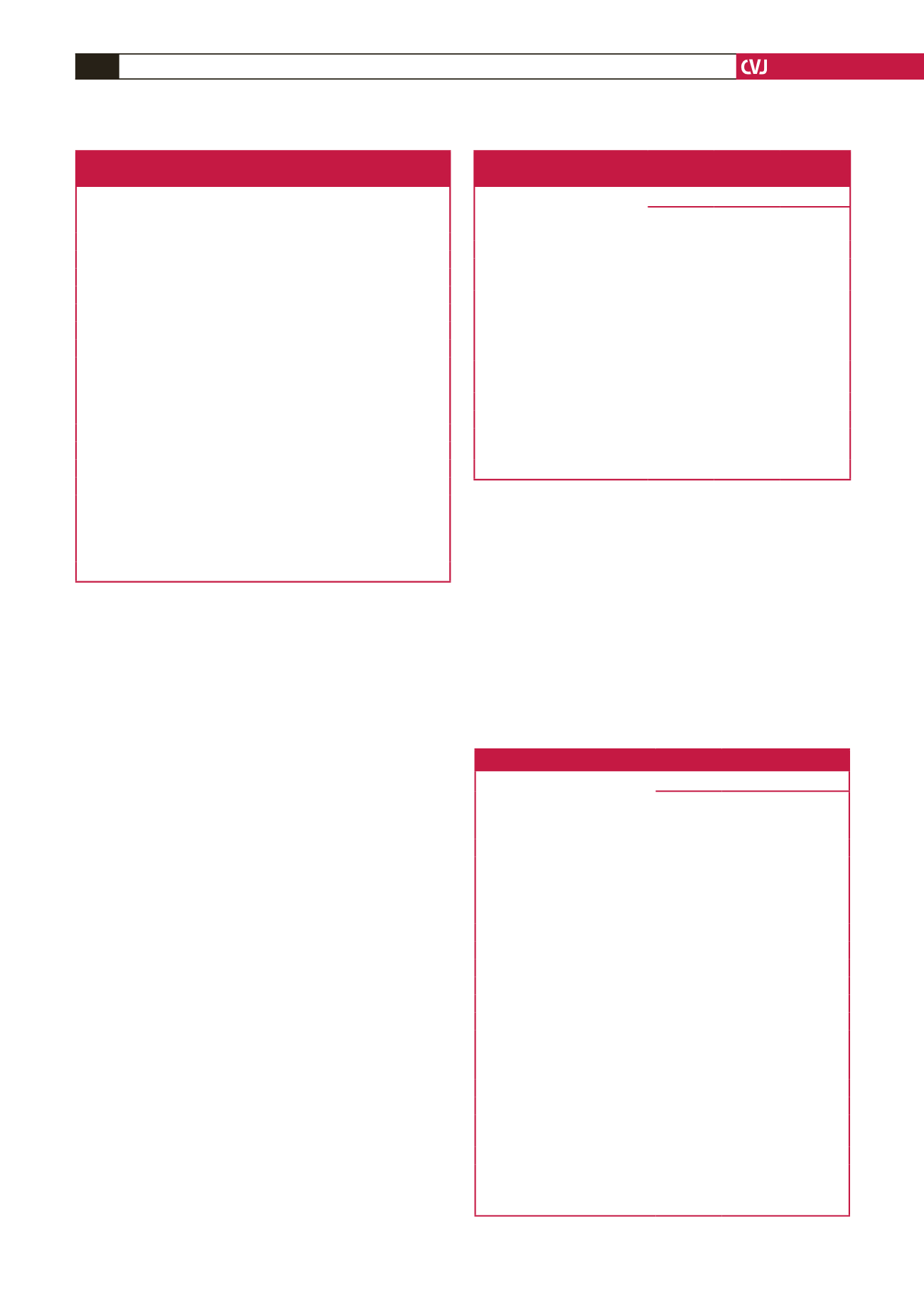
Table 4. Risk factors for thromboembolism among
patients on admission
Risk factor
Number (%) of patients
Surgical
(
n
=
1016)
Medical
(
n
=
567)
All patients
(
n
=
1583)
Previous VTE
3 (0.3)
2 (0.4)
5 (0.3)
Chronic pulmonary disease
(CPD)
21 (2.0)
45 (8.0)
66 (4.2)
Obesity
104 (10.2) 59 (10.4) 163 (10.3)
Thrombophilia
–
2 (0.4)
2 (0.1)
Long-term immobility
44 (4.3)
41 (7.2)
85 (5.4)
Contraceptive
10 (1.0)
–
10 (0.6)
Varicose veins or venous
insufficiency (VVI)
17 (1.7)
7 (1.2)
24 (1.5)
Pregnancy
81 (8.0)
1 (0.2)
82 (5.2)
Chronic heart failure
13 (1.3)
95 (16.8)
108 (6.8)
Post-menopausal hormone
replacement therapy
–
1 (0.2)
1 (0.1)
None
764 (75.2) 354 (62.4) 1118 (70.6)
Table 5. Patients presenting with more than one risk factor
Risk factor
Number (%) of patients
Surgical
(
n
=
1016)
Medical
(
n
=
567)
All
patients
(
n
=
1583)
CPD + obesity
5 (0.5)
1 (0.2)
6 (0.4)
Previous VTE + obesity + VVI
+ CHF
–
1 (0.2)
1 (0.1)
CPD + long-term immobility
1 (0.1)
–
1 (0.1)
CPD + pregnancy
1 (0.1)
–
1 (0.1)
Obesity + long-term immobility 2 (0.2)
3 (0.5)
5 (0.3)
Obesity + VVI + CHF
1 (0.1)
–
1 (0.1)
Obesity + VVI
4 (0.4)
1 (0.2)
5 (0.3)
Obesity + pregnancy
23 (2.3)
–
23 (1.4)
Long-term immobility + VVI
3 (0.3)
1 (0.2)
4 (0.2)
CPD + obesity + CHF
–
1 (0.1)
1 (0.1)
CPD + long-term immobility
+ CHF
–
2 (0.3)
2 (0.1)
CPD + VVI + CHF
–
1 (0.1)
1 (0.1)
CPD + CHF
–
10 (1.8)
10 (0.6)
Obesity + CHF
–
5 (0.9)
5 (0.3)
Thrombophilia + long-term
immobility + CHF
–
1 (0.1)
1 (0.1)
Long-term immobility + CHF
–
5 (0.9)
5 (0.3)
VVI + CHF
–
1 (0.2)
1 (0.1)
CPD: chronic pulmonary disease, CHF: chronic heart failure, VVI:
varicose veins or venous insufficiency.