
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 5, September/October 2014
AFRICA
215
ADMA is an endogenous NOS inhibitor competing with
L-arginin to bind to NO. The plasma ADMA level was reported
to be elevated in coronary artery disease and it is seen to be a risk
factor with a worse clinical outcome for percutaneous coronary
interventions.
26-28
Studies have consistently indicated that cardiac
I/R caused elevation in levels of serum ADMA
29
and myocardial
tissue ADMA.
30
In our study, tissue ADMA levels were elevated
with I/R, which was reduced in the rosuvastatin group.
Elevated NADPH levels lead to elevation in ROS levels and
decreased bioavailability.
7
NADPH oxidase activity was reported
to increase in the heart with I/R. NADPH oxidase was shown to
be related to platelet activation and thrombus formation in I/R.
8
In our study, the NADPH oxidase level increased with I/R and
this elevation decreased with rosuvastatin administration.
Pignatelli
et al
.
8
demonstrated that rosuvastatin caused
antiplatelet activity independent of its lipid-lowering effect
and this was related to its effect of reducing NADPH oxidase
levels. In the same study, rosuvastatin was shown to reduce
oxidative stress by reducing NADPH oxidase levels, upregulating
antioxidant enzymatic defence mechanisms and inhibiting
hydrogen peroxide-mediated DNA damage.
Hsp 90 is a cytoprotective protein chaperone that participates
in mitochondrial import of a number of proteins. It was
shown to increase I/R-related necrotic cell death when blocked
pharmacologically.
31
Hsps are reported to be protective by being
upregulated in the case of increased oxidative stress.
32
Under our
experimental conditions, the hsp 90 level was seen to increase as
a protective mechanism during I/R. We believe that the expected
increase in hsp 90 levels would not have been seen together with
the decrease in injury due to the positive effects of rosuvastatin
on the other parameters.
Caveolin-1 elevation has been shown to contribute to the
pathology of cardiovascular diseases, and caveolin-1 peptide
was reported to be protective for the heart in myocardial I/R.
This effect involved a NO-mediated mechanism.
14
Caveolin-1
deficiency was shown to aggravate cardiac dysfunction and
reduced survival rate in rats that experienced MI.
15
Although
a significant change was not detected in caveolin-levels in our
study, other studies are available indicating that myocardial
caveolin-1 content decreased following I/R.
14
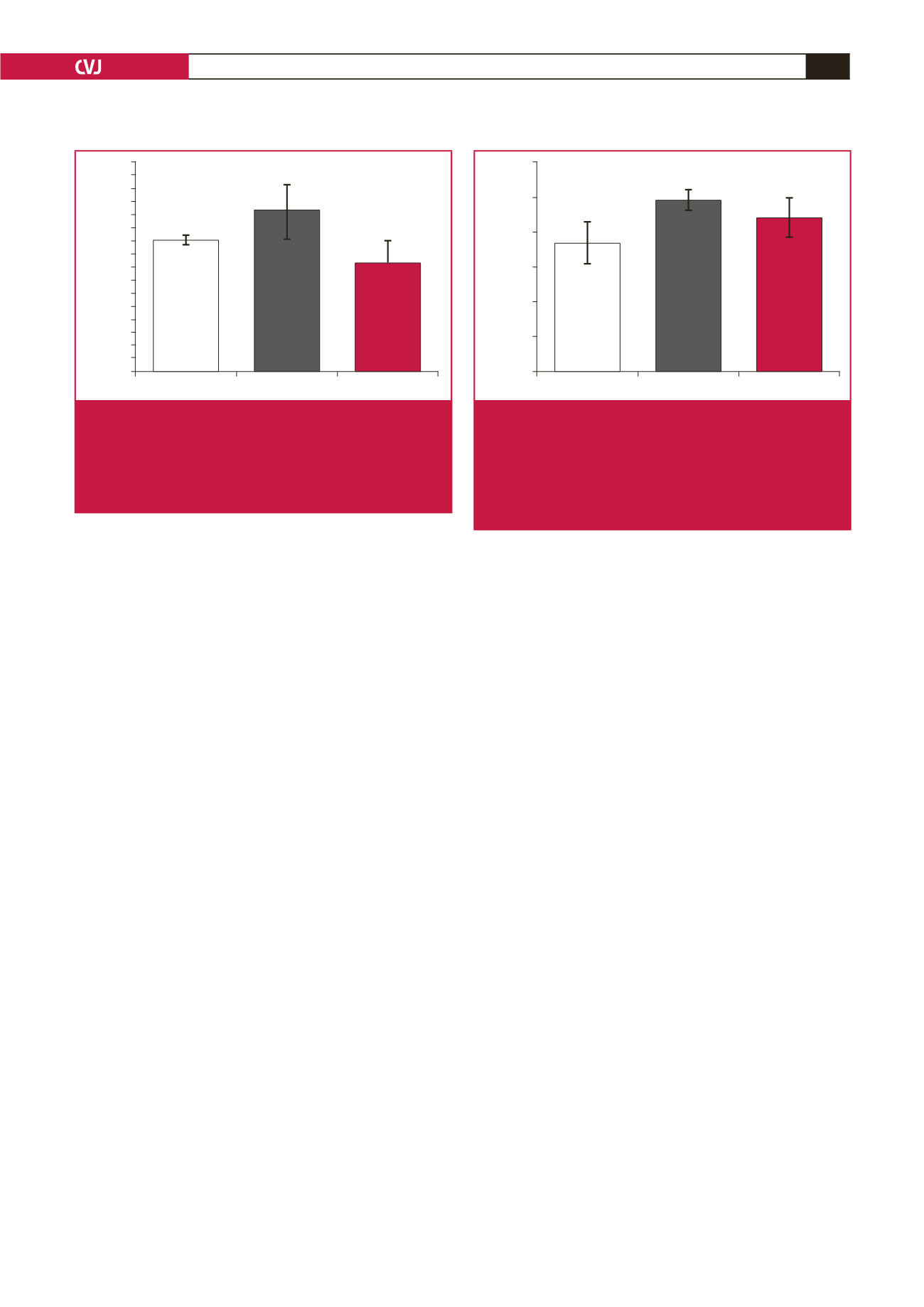
In this experimental study, rhokinase levels were detected
to increase following I/R. Rhokinase activity has been shown
to increase during reperfusion and played an important role in
I/R-related myocardial injury.
33
Animal studies have suggested
that rhokinase inhibition protects the heart against I/R injury.
Administration of the rhokinase inhibitor, Y-27632, significantly
inhibited rhokinase activation in I/R and reduced the infarct
area.
33
In the present study, rhokinase activity was observed
to decrease when rosuvastatin was administered. Similarly,
rhokinase activity could be inhibited in long-term administration
of rosuvastatin and in cell cultures.
34-36.
NFkB is a redox-sensitive transcription factor that is
activated in response to oxidative stress and is responsible for
the production of inflammatory genes. Reduction in sensitivity
to I/R injury in NFkB knock-out mice suggested that NFkB-
mediated inflammatory responses play an important role in
injury.
37
The area of the myocardial infarct induced by reperfusion
decreased significantly when NFkB activation was blocked
through PS-519.
38
Results of the study showed that reperfusion
injury may be inhibited when NFkB activation is suppressed. In
the present study, NFkB levels significantly increased with I/R.
This increase was significantly reduced when rosuvastatin was
administered, and the levels returned to control values.
Conclusion
The effect of chronic administration of rosuvastatin on
oxidative stress, inflammation and endogenous NO generation
in I/R injury has been reported for the first time in our study.
Rosuvastatin caused inhibition of I/R-mediated increases in
related mediators, although not significantly for ADMA and
NADPH oxidase levels. We believe that rosuvastatin may be
important in treatment protocols of myocardial I/R due to its
positive effects on rhokinase, NADPH oxidase, ADMA, hsp 90
and NFkB levels, although further studies are necessary.
160
150
140
130
120
110
100
90
80
70
60
50
40
30
20
10
0
Control
IR
Rosuvastatin
Rhokinase level (ng/ml)
Fig. 5.
Effect of rosuvastatin on rhokinase levels in myocar-
dial I/R. Vehicle or rosuvastatin (10 mg/kg) were
administered by intraperitoneal injection for 15 days
before ischaemia (
n
=
7 in each group). a;
p
<
0.05
significantly different from IR group (one-way analysis
of variance followed by a
post hoc
Tukey HSD test).
6000
5000
4000
3000
2000
1000
0
Control
IR
Rosuvastatin
NADPH Oxidase level (pg/ml)
Fig. 6.
Effect of rosuvastatin on NADPH oxidase levels in
myocardial I/R. Vehicle or rosuvastatin (10 mg/kg)
were administered by intraperitoneal injection for 15
days before ischaemia (
n
=
7 in each group). *
p
<
0.05 significantly different from control group (one-way
analysis of variance followed by a
post hoc
Tukey
HSD test).



















