
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 5, September/October 2014
218
AFRICA
Methods
The Abeokuta HF registry was a hospital-based, single-centre,
prospective, observational study that consecutively recruited 285
subjects with
de novo
AHF and 24 cases of decompensated HF
(acute-on-chronic HF), all admitted during the period 1 January
2009 to 31 December 2010. The 24 cases of decompensated HF
were excluded from the final analysis.
The main objective of the registry was to characterise the
current profile of HF in the community. It was also aimed at
determining the mode of care as well as intra-hospital and
six-month outcomes.
Clinical information relating to the socio-demography, medical
history, signs and symptoms, medications, results of laboratory
investigations, including 12-lead ECG and echocardiography,
were collected. A standardised case report form was used for
data collection. Home addresses and telephone contacts of the
subjects as well as their next of kin were also recorded.
Subjects were weighed without shoes and in light clothing
using a standard beam balance. An anthropometric plane was
used for height measurement to the nearest centimetre. Bodymass
index (BMI) was calculated using the standard formula. Blood
pressure measurements were done according to international
guidelines,
15
with the use of a mercury sphygmomanometer
(Accousson, London).
We defined anaemia as haematocrit of less than 10 g/dl. The
modification of diet in renal disease (MDRD) formula was used
for the estimation of glomerular filtration rate (GFR).
16
An
estimated GFR (eGFR) of less than 60 ml/min/1.73 m
2
was the
criterion used for defining renal dysfunction.
4
A clinical diagnosis of HF was based on the Framingham
criteria.
17
Using the recent guidelines of the European Society of
Cardiology,
18
subjects were categorised into
de novo
presentation,
as well as recurrent presentation of typically decompensated HF
(i.e. acute-on-chronic HF).
Standard 12-lead resting ECGs were recorded for each patient
using a Schiller ECG machine (Schiller AG, Switzerland). All
the 12-lead resting ECGs were performed by trained nurses/
technicians and analysed by a reviewer who was blinded to the
clinical data of the patients.
Echocardiography was performed on the subjects with the
use of an Aloka SSD – 4000 echocardiography (Aloka Co Ltd,
Tokyo, Japan). Standard views and two-dimensional guided
M-mode measurements were obtained according to international
guidelines. Aortic root and left atrial diameter, left ventricular
(LV) internal dimensions and wall thicknesses were obtained
according to the American Society of Echocardiography (ASE)
criteria. Measurements were obtained in up to three cycles and
averaged. One experienced cardiologist (OSO) performed all the
procedures.
In our laboratory, the intra-observer concordance correlation
coefficient and measurement errors have been reported.
19
The Devereux and Recheck formula was used for LV mass
calculation.
20
Increased relative wall thickness (RWT) was
defined as RWT > 0.43.
21
Impaired LV systolic function was defined as LV ejection
fraction of
<
50%. Transmitral flow velocities, deceleration
time and isovolumic relation time were obtained using standard
methods.
22
Tissue Doppler imaging (TDI) was applied only to
identify true pseudo-normalised filling pattern.
The cohort was prospectively followed up for six months. The
mean follow-up period was 205 days. Subjects were contacted
via clinic visits or telephone calls at one, three and six months.
Follow-up data included their wellbeing, medications, history
of rehospitalisation and deaths (from next of kin). In addition
to patient or relative telephone interviews, where necessary,
referring physicians were contacted for additional information.
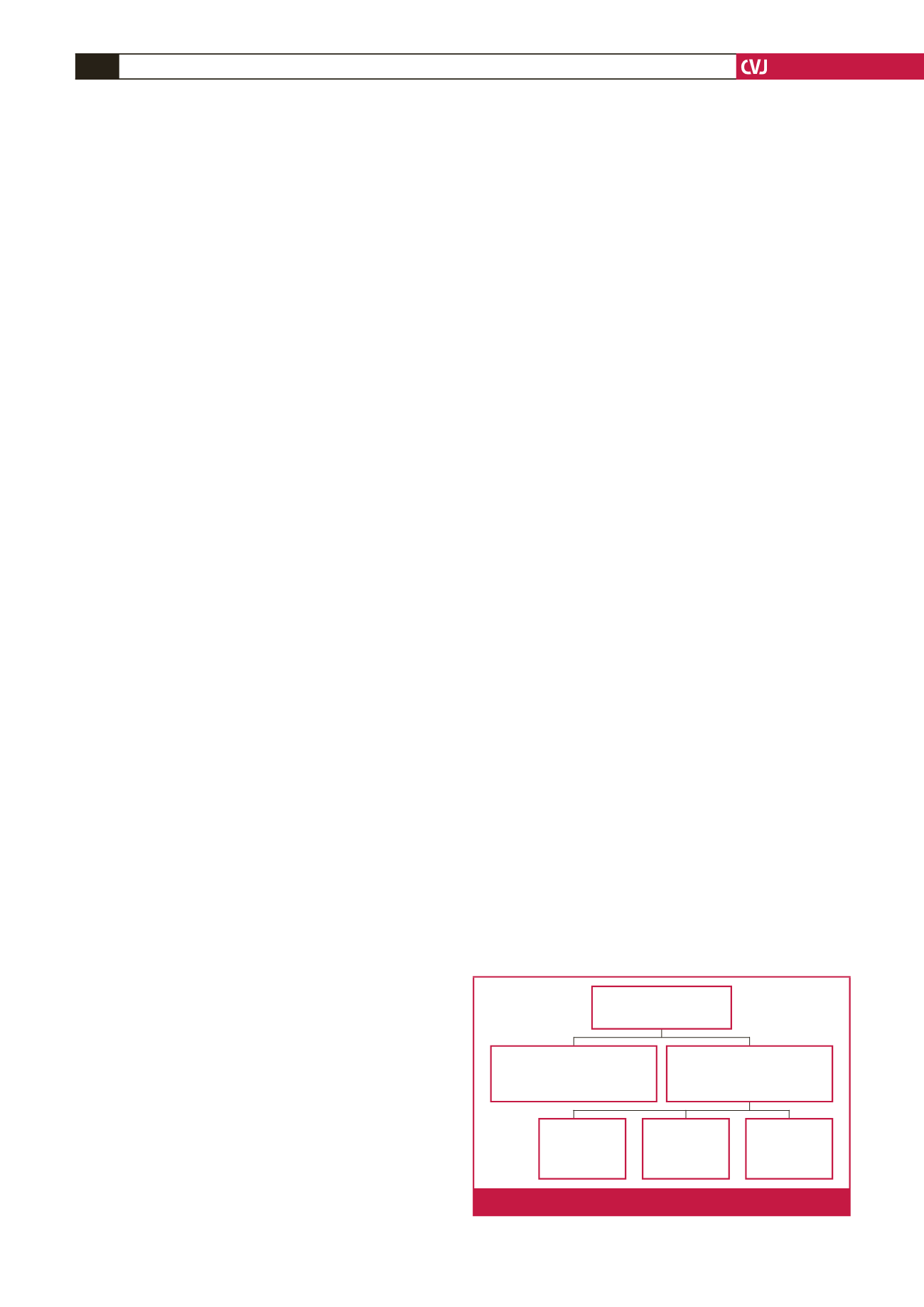
Fig. 1 is a flow chart showing the recruitment and follow up of
the study cohort.
We examined (1) length of hospital stay (LoS), (2) Survival
status on discharge (dead or alive), (3) short-term case fatality/
re-admission (30 days), (4) medium-term case fatality (within
180 days), (5) rehospitalisation status (within 180 days), and (6)
event-free survival from re-admission or death.
The study was reviewed and approved by the institution’s
ethics review board. All the subjects gave informed consent and
the study was carried out in accordance with the Declaration of
Helsinki.
23
Statistical analysis
Data were entered into EpiData software. The EpiData
association (att. Jens Lauritsen, Enghavevej 34, DK5230 Odense
M, Denmark) was used for data entry, while SPSS version 15
and Stata version 11.1 were used for data cleaning and analysis.
Continuous variables are presented as means and standard
deviations (SDs), or medians with their 25th and 75th percentiles
when the distribution of the data did not follow Gaussian
distribution.
Categorical variables are displayed as frequencies and
proportions. Group comparison was done with the Student’s
t
-test, and chi-square statistics were used for comparison of
categorical variables. Survival function estimates were performed
using the Kaplan–Meier method and the difference was tested
using the log-rank test. The follow up was censored at six months
post admission.
Predictors of survival were determined using univariate
regression analyses. Thereafter multiple logistic regression
analysis was performed to identify independent predictors of
survivals (
p
<
0.1 used for selection of variables).
Results are expressed as odds ratio (OR) with their 95%
confidence intervals (95% CI). Odds ratios that were significantly
greater than 1.00 implied that subjects with that attribute had
higher risks of death compared to subjects who did not. A
p
-value of
<
0.05 was taken as significant.
309 consecutive AHF
subjects recruited
242 subjects
were known
to be alive
23 subjects
were known
to have died
20 subjects
were lost to
follow up
24 decompensated (acute-
on-chronic HF) cases
excluded from the analysis
285
de novo
AHF cases
included in the analysis
Fig. 1.
Flow chart showing the recruitment of the subjects.



















