
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 5, September/October 2014
AFRICA
247
rate to be 13%, which was increased to 24% with combined
surgery.
13
In our study, in-hospital mortality was 8.7% in patients
with isolated AVR and 16.7% in patients with combined surgery.
In addition, early reports in the elderly have shown mortality
rates of 2–10% for isolated AVR.
14,15
Concomitant CABG was also identified as an independent
predictor in a clinical series.
16
However, in a study including 450
patients aged
≥
80 years, Unic
et al
.
17
showed that concomitant
CABG did not affect the late survival rate.
In our study, we did not find any correlation between
combined surgery and mortality rate. Even though LMCA
stenosis, NYHA
≥
III and EuroSCORE
≥
15 were associated
with early mortality in the univariate analysis, multivariate
logistic regression analysis revealed that the only risk factor
associated with surgical mortality was CBP time, as anticipated.
In other words, simple operations with shorter CPB times may
be more beneficial than better complex operations with longer
CPB times in high-risk patients.
In addition, our study findings confirmed that patients
undergoing combined surgery with concomitant CABG showed
lower long-term survival rates compared to surgical mortality
rates, from 16.7% post operatively to 13.3% long-term survival.
This is noticeably lower than the 24% early mortality that
was reported by Kolh
et al
.
18
Kurlansky
et al.
16
also identified
concomitant CABG as a predictor of mortality; however, they
showed the improvement in quality of life in the long term.
In our study, mitral valve surgery was associated with an
increased mortality rate (30.1%). This was consistent with a
number of previous studies.
15,19
It has been reported that AVR
can be performed in elderly patients with an acceptable mortality
rate, high long-term survival rate and functional improvement.
14,20
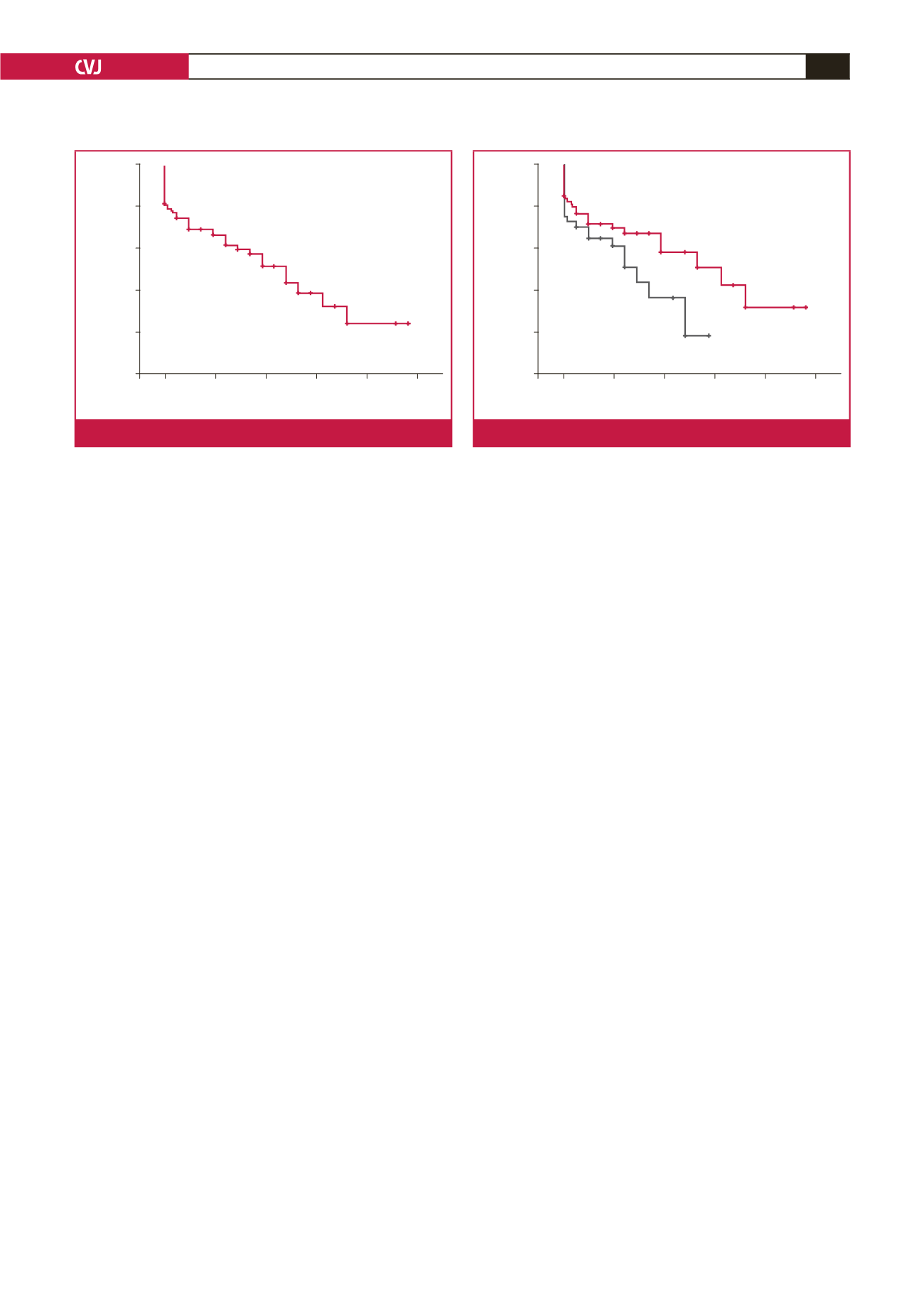
One-, three- and five-year survival rates were 76.2
±
4.12, 69.03
±
4.44 and 61.40
±
5.13%, respectively. However, these rates need
to be confirmed.
13,14
The low survival rates in our study can be attributed to
multiple factors, including that 87.7% of patients had extracardiac
co-morbidities; 10.5% had poor ejection fraction, and 86% were in
NYHA class
≥
III. Postoperative pacemaker, respiratory infection
and haemodialysis were predictors for late mortality, while aortic
cross-clamp time and CPB time were found with multivariate
analysis to be independent predictors of mortality. These results
suggest that combined surgery entails prolonged ischaemic time,
leading us to tailor an appropriate surgical strategy for each patient.
The use of bioprosthetic valves, which allow for implantation
of larger prostheses, was lower than in previous studies. The
early experiences of Peterseim
et al
.
21
reported that bioprostheses
should be considered in patients with a number of co-morbidities
or aged
≥
65 years. In a retrospective study, however, Silberman
et al
.
22
reported that the selection of valve replacement device
should be based on life expectancy, patient preference, lifestyle
and surgery-related complications.
The limitations of the present study include missing
information due to limited data collection, as it was a retrospective
study, and missed regular out-patient visits. Although 98.9% of
patients completed the follow-up period, less attention was paid
to the quality of life. Among long-term survivers, only two
patients had poor activity levels. However, the Short form 36
health survey should be completed for further investigation of
long-term quality of life.
Conclusion
It is obvious that we need more surgical experience on elderly
patients. Our study results demonstrate that an individually
tailored approach including scheduled surgery increased short-
and long-term outcomes of AVR in patients aged
≥
70 years.
In addition, shorter cardiopulmonary bypass time may be more
beneficial in this high-risk patient population.
Although several issues should be considered for elderly
patients undergoing cardiac surgery, including socio-economic
factors, the possible benefits of surgery should not be ignored
in patients with aortic valve disease who are eligible for surgery.
In addition, in the presence of combined cardiac procedures, a
hybrid approach or transcatheter aortic valve implantation with
isolated conventional AVR may be an alternative in high-risk
patients.
References
1.
HALE (healthy life expectancy 2000–2011) World Health Organization,
http://www.who.int/healthinfo/statistics/indhale/en.2.
Sedrakyan A, Vaccarino V, Paltiel AD, Elefteriades JA, Mattera JA,
Roumanis SA,
et al
. Age does not limit quality of life improvement in
cardiac valve surgery.
J Am Coll Cardiol
2003;
42
: 1208–1214.
1.0
0.8
0.6
0.4
0.2
0.0
0
50 100 150 200 250
Follow up (month)
Probability of survival
Fig. 1.
Probability of survival.
1.0
0.8
0.6
0.4
0.2
0.0
0
50 100 150 200 250
Follow up (month)
Probability of survival
Fig. 2.
Survival rates in the combined surgery group.



















