
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 5, September/October 2014
e2
AFRICA
The patient was weaned uneventfully from CPB without
inotropic support. The postoperative course was uneventful and
the patient was discharged on the sixth postoperative day.
At the one-year follow up, the patient reported an active life.
Echocardiography revealed an ejection fraction of 53% and
satisfactory LV remodelling.
Discussion
LV pseudo-aneurysm develops when a free-wall rupture is
contained by overlying adherent pericardium.
4
A small, narrow-
necked channel connects the LV with the sac. A LV pseudo-
aneurysm does not contain an endocardial or myocardial layer
of the LV wall.
5
By contrast, a true LV aneurysm is a result of the
thinning of the LV wall due to scar formation after MI.
Pseudo-aneurysms may lead to fatal rupture at any time after
MI, or to arrhythmia, cardiac dysfunction or emboli.
6
Eren
et al
.
reported the rate of incidence of pseudo-aneurysms between 31
and 45%.
1
The most common cause of pseudo-aneurysms is an MI due
to the occlusion of the right coronary or LAD artery.
7
One-third
of pseudo-aneurysms are due to a complication of cardiac
surgical procedures, mostly mitral valve replacement.
5
Other
aetiological factors are infection and trauma.
3
LV pseudo-aneurysms are usually asymptomatic, and
are recognised on investigation for other conditions, mostly
congestive heart failure (36%), chest pain (30%) or dyspnoea
(25%).
5
Other presentations are arrhythmia and embolisation.
1
Our patient had a history of anterior MI, and hence the
complaint of dyspnoea at rest and palpitations as symptoms of
congestive heart failure.
Computed tomography, echocardiography and magnetic
resonance imaging are helpful in the pre-operative diagnosis
but coronary angiography and contrast ventriculography
are necessary to evaluate the coronary arteries and precise
localisation of the pseudo-aneurysm.
The timing of surgery depends on time since the MI. Urgent
surgical repair is recommended if the pseudo-aneurysm is
detected early after MI because of the risk of rupture.
8
The
rate of incidence of cardiac rupture in untreated pseudo-
aneurysms ranges from 30 to 45%.
5
However, with chronic
pseudo-aneurysms, the symptoms are more important than the
risk of rupture in determining the necessity of operation.
9
Yeo
et al
. treated 10 patients with pseudo-aneurysm
conservatively and in none of the cases was cardiac rupture
documented after a median follow up of 2.3 years.
10
Moreno
and colleagues treated nine patients with LV pseudo-aneurysm
conservatively and reported a cumulative survival of 88.9
and 74.1% at one year and four years, respectively.
4
The rate
of incidence of mortality after surgical repair of LV pseudo-
aneurysms ranges from 13 to 29%.
4
The rate of intra-operative and post-operative complications
due to the use of CPB and cardioplegic arrest is low in low-risk
patients, but the scenario is different when the technique is
applied to high-risk groups, or patients requiring emergency
surgery.
11
Complications related to conventional CPB are due
to the release of inflammatory mediators, the administration of
cardioplegia, aortic cross-clamping and hypothermia.
12
On the other hand, the off-pump technique can cause
episodes of transitory haemodynamic deterioration that could
result in inadequate coronary artery blood flow, followed by
severe complications or death.
13
Perrault
et al
. proved that the
ONCAB/BH technique, which represents the idea of using CPB
without cross-clamping and cardioplegic arrest, with the heart
beating, can be effectively used in high-risk patients who cannot
tolerate cardioplegic arrest, and is associated with less myocardial
oedema and ischaemia.
14
The benefits of this technique are the
absence of cardioplegic arrest (global myocardial ischaemia
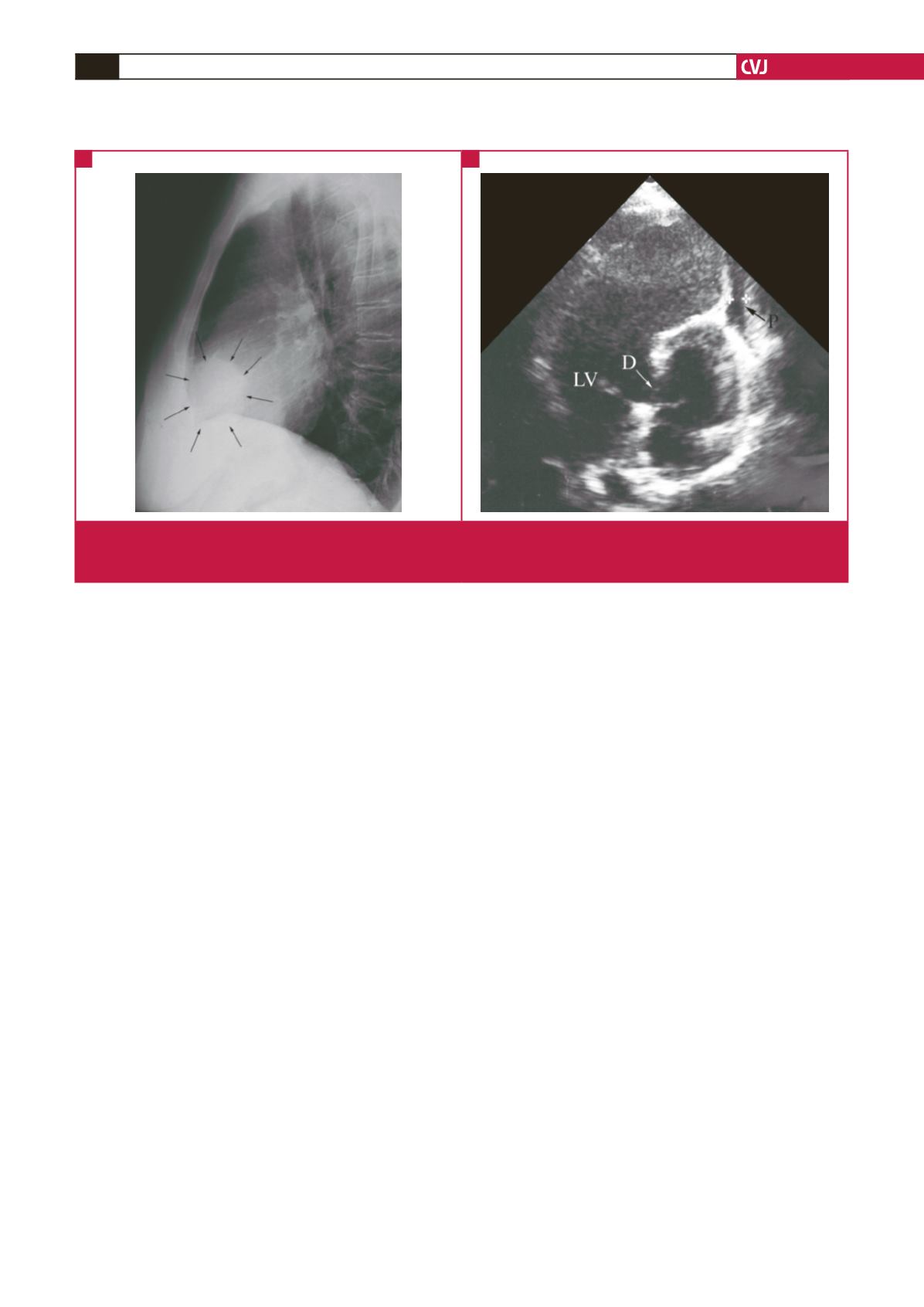
Fig. 1. (A) Pre-operative chest X-ray (lateral projection) visualising the aberrant contour of the LV pseudo-aneurysm.
(B) Pre-operative transthoracic echocardiography demonstrating the anterolateral pseudo-aneurysm (LV: left ventricle,
D: defect, P: pericard).
A
B



















