
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 5, September/October 2014
AFRICA
e3
during aortic cross-clamping time followed by reperfusion) and
the reduction in haemodynamic instability caused by extensive
surgical manipulation of the heart.
Patients presenting with LV pseudo-aneurysm are usually
high-risk patients with low ejection fraction. Our patient’s
pre-operative ejection fraction was 32%. As we achieved complete
revascularisation in our patient, ONCAB/BH eliminated the
difficulty of grafting the circumflex and posterior descending
coronary arteries. We performed longitudinal plication before
resection of the necrotic muscle to prevent air embolism as well
as to provide clear and bloodless surgical exposure.
Conclusion
The rare but fatal complication of MI, LV pseudo-aneurysm,
can be surgically repaired using the on-pump beating heart and
longitudinal plication technique so that the patient does not
develop LV thrombus.
References
1.
Eren E, Bozbuga N, Toker ME, Keles C, Rabus MB, Yildirim O,
et al.
Surgical treatment of post-infarction left ventricular pseudoaneurysm: a
two-decade experience.
Tex Heart Inst J
2007;
34
(1): 47–51.
2.
Pollak H, Nobis H, Miczoc J. Frequency of left ventricular free wall
ruptures complicating acute myocardial infarction since the advent of
thrombolysis.
Am J Cardiol
1994;
74
: 184–186.
3.
Prêtre R, Linka A, Jenni R, Turina MI. Surgical treatment of acquired
left ventricular pseudoaneurysms.
Ann Thorac Surg
2000;
70
: 553–557.
4.
Moreno R, Gordillo E, Zamorano J, Almeria C, Garcia-Rubira JC,
Fernandez-Ortiz A,
et al
. Long term outcome of patients with postin-
farction left ventricular pseudoaneurysm.
Heart
2003;
89
(10): 1144–1146.
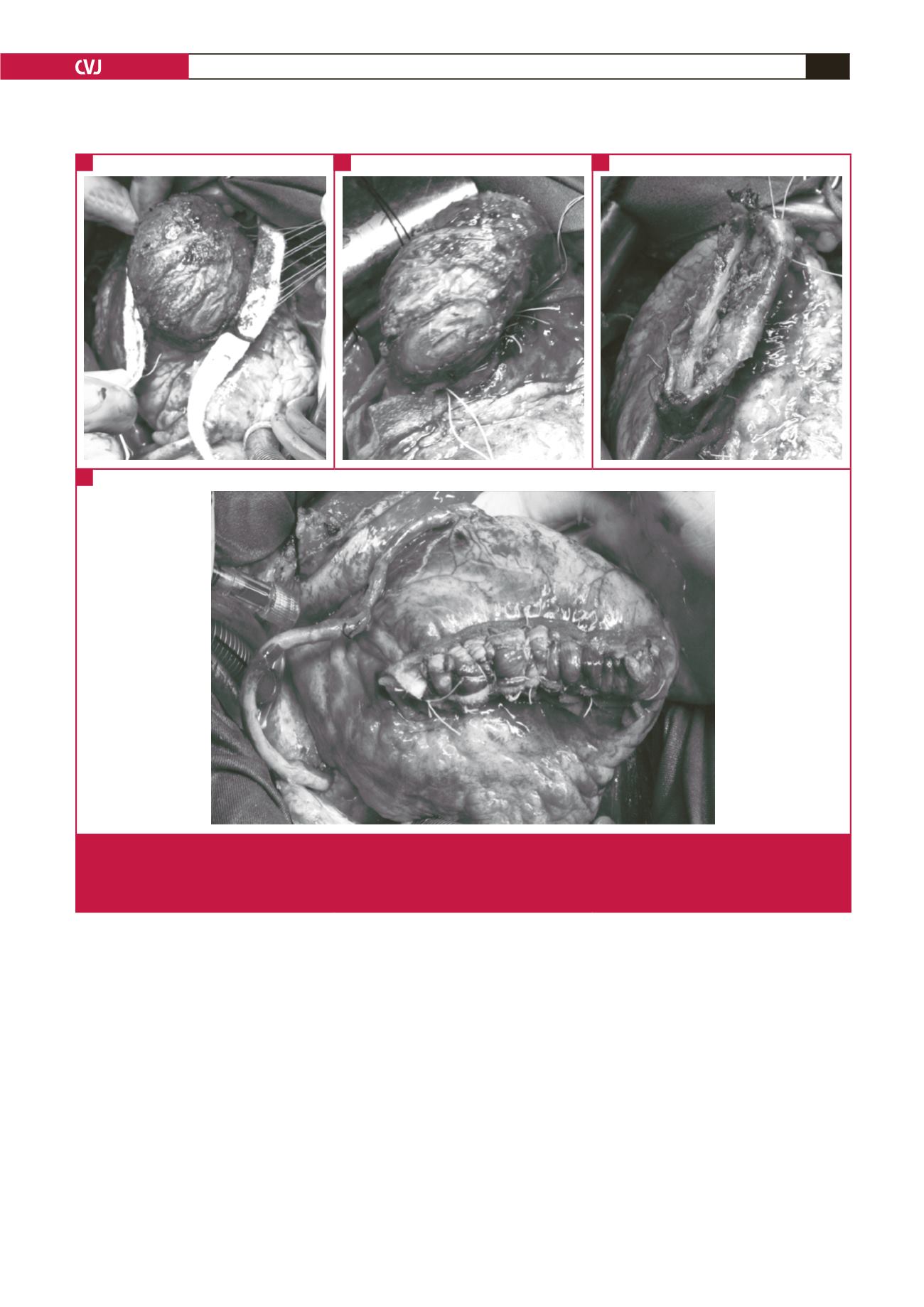
Fig. 2. (A) Full-thickness U sutures (0 Ethibond) passed from strips of Teflon and stable endocardium. (B) Longitudinal plication line,
which was buttressed by Teflon felt strips. (C) The necrotic part of the left ventricular wall was removed. (D) The plication was
strengthened with sutures and sequential coronary artery bypass venous grafting was performed to the first diagonal branch
of the left anterior descending artery and the first obtuse marginal branch of the circumflex artery.
A
D
B
C



















