CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 1, January/February 2016
AFRICA
47
(other abnormalities generally presenting much earlier).
Congenital heart and vascular defects that have been described
include dextrocardia with situs inversus totalis (mirror image),
situs solitus with normal relationship of great arteries (variation
of dextroversion), situs solitus with levo- and/or dextro-
transposition of the great arteries, and dextrocardia associated
with polysplenia syndrome.
2
Dextrocardia can also be associated with the heterotaxy
syndromes of asplenia and polysplenia. Of the two syndromes,
polysplenia is more likely to be associated with less severe cardiac
malformations and therefore more likely to be encountered
in adults. Up to 50% of cases of polysplenia syndrome can
have dextrocardia. In polysplenia syndrome, there tends to be
non-cyanotic congenital heart defects.
2
Abnormalities associated with polysplenia syndrome are
bilaterally symmetrical liver, bilateral bi-lobed lungs with bilateral
hypo-arterial bronchi (left isomerism), bilateral superior vena
cava, absence of the intrahepatic portion (interruption) of the
inferior vena cava with azygous or hemi-azygous continuation,
common atrium with complete absence of the atrial septum,
endocardial cushion defect, hypoplasia or absence of one
ventricle, valvular or subvalvular pulmonary stenosis, aortic
stenosis or atresia, and double-outlet right ventricle. There
is also an unexplained relationship between polysplenia and
Kartagener’s syndrome.
2
Left ventricular non-compaction (LVNC) is a hereditary
primarycardiomyopathywithcharacteristicfeaturesof prominent
trabeculations and conspicuous inter-trabecular recesses that
penetrate deeply into the left ventricular myocardium, with a
thin, compacted ventricular free wall (mainly in the affected
areas), and diffuse systolic dysfunction with hypokinesia.
5
The
majority of reported cases describe involvement of the left
ventricle, but the right ventricle and septum can also be affected.
6
Non-compaction of the ventricular myocardium was first
described in 1932, in an autopsy on a newborn.
7
Since then, due
to increasing awareness and continuously improving technology,
the rates of diagnosis of LVNC have been steadily increasing.
Imaging studies are the cornerstone of diagnosis of LVNC, with
echocardiography being the main diagnostic tool. Computed
tomography, angiography and magnetic resonance imaging
(MRI) have been and can be used with equal success at
diagnosis of the entity as well as for identification of associated
abnormalities.
In the normally developed heart, the left ventricle has up to
three prominent trabeculations and is less trabeculated than the
right ventricle. In LVNC the trabeculations are more numerous
(left ventricle compared to right ventricle) and thicker with deep
recesses between the trabeculae.
Several diagnostic criteria have been proposed for LVNC,
including a ratio of two for the wall thickness between the
non-compacted trabeculated layer and the non-trabeculated
compacted layer of the LVNC at end-systole, as measured
along the parasternal short axis on echocardiography.
8
Other
criteria that can be used for diagnosis and possible classification
include:
8
(1) prominent and deep inter-trabecular recesses in the
left ventricular lateral wall and apex, (2) direct blood flow from
the ventricular cavity into the deep inter-trabecular recesses,
as assessed by Doppler echocardiography, (3) two-layered
structure of the ventricular wall, with an end-systolic ratio of
non-compacted-to-compacted layer exceeding 1.4 (in infants),
and (4) absence/presence of co-existing cardiac abnormalities.
The clinical presentation can vary and initially most children
and adults are asymptomatic. The left ventricular function then
gradually deteriorates and other presenting events may also
occur, such as cardiac failure and thromboembolic events. The
prognosis is poor, with patients facing the possibility of sudden
death (due to cardiac arrhythmias, ischaemic strokes, etc.) or
eventual death due to heart failure.
9
The systolic dysfunction is thought to occur due to a relative
ischaemia of the myocardium with a mismatch of myocardial
oxygen supply and demand.
6
Restricted myocardial perfusion
and decreased coronary flow reserve, which suggests a coronary
microcirculatory dysfunction, has been demonstrated previously
by Jenni
et al
. with positron emission tomography (PET)
10
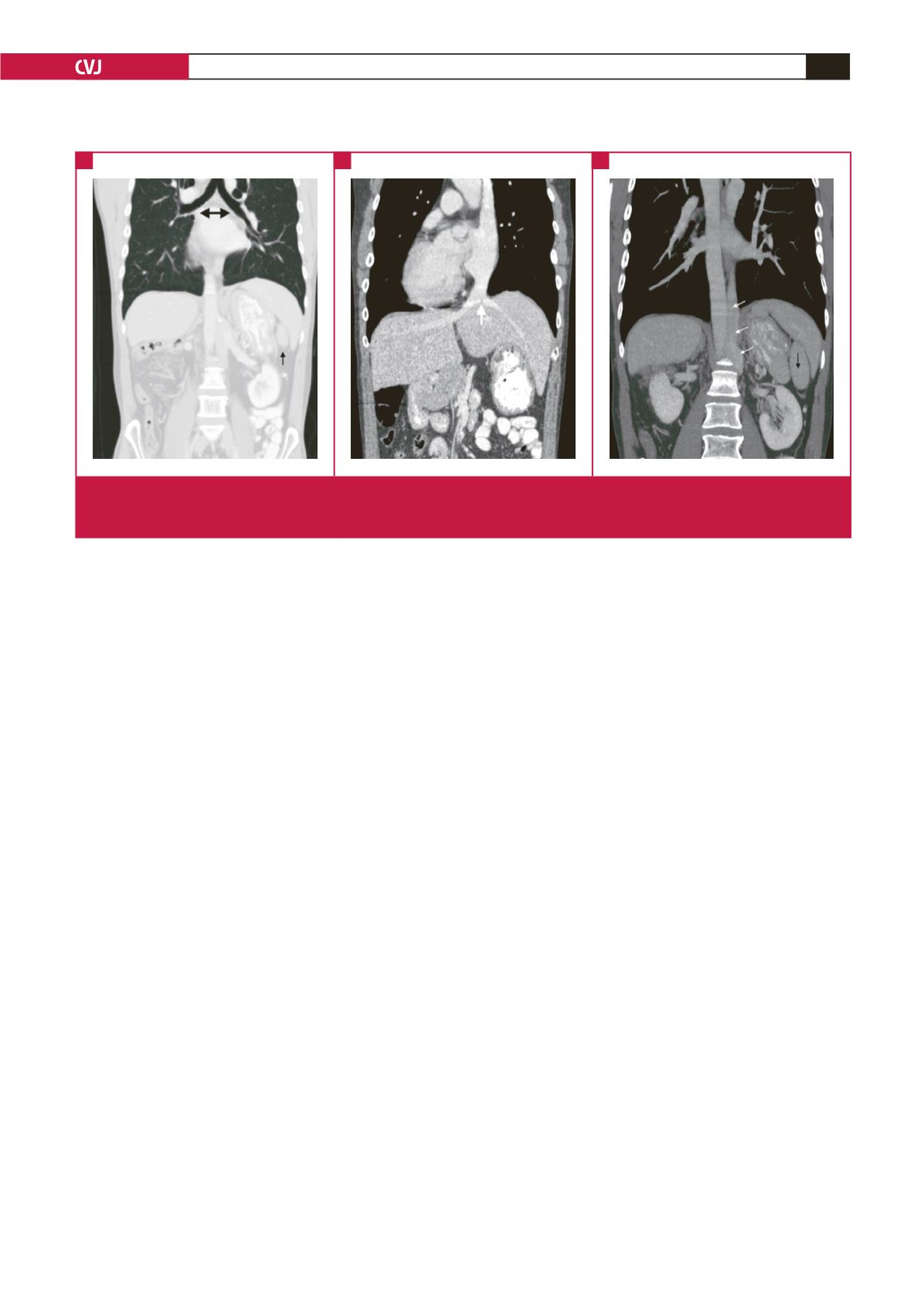
Fig. 3.
Computed tomography angiogram (coronal slices) with lung window (A) and venous phases (B) and (C). Splenule (small
black arrow), bilateral hypo-arterial bronchi (black double arrowheads), interruption of the inferior vena cava (larger white
arrow) and azygous continuation of the inferior vena cava (small white arrows) are all part of the heterotaxy syndrome.
A
B
C

















