
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
AFRICA
69
Discussion
This study describes, perhaps for the first time, the use of
postpartum ECG variables in a simple risk score that seems
to predict PPCM diagnosis among women at risk for the
disease. PPCM patients and controls had similar age, systolic
and diastolic blood pressures and body mass index. Therefore,
the findings could not have been influenced by these possible
confounders.
Our findings show that the presence of heart rate less than 100
beats/min reduced the risk of diagnosing PPCM to 89.7%, while
the presence of ST–T-wave abnormalities, QRS duration more
than 110 ms and QTc duration longer than 460 ms increased
the odds of PPCM 12.0-, 5.2- and 9.5-fold, respectively. In the
initial multiple regression model, heart rate and ST–T-wave
abnormalities maintained their high statistical significance in
predicting PPCM but not QRS duration and QTc interval. This
finding was not influenced by serum sodium or potassium levels.
None of our patients had malignant arrhythmia, and ectopic
beats were equally uncommon in both groups. These results are
supported by previous reports in women with PPCM as well as
in healthy pregnant women.
3,12
Serum sodium and potassium levels were significantly lower
in the patients than the controls, possibly because of water
retention caused by heart failure syndrome.
7
It should be noted
that patients were all recruited at the time of confirmation of the
diagnosis, when most heart failure treatments were commenced,
and none was on drugs that could affect ECG measurements.
For the first time, we have developed a simple scoring system
using three ECG variables that could potentially predict PPCM
with an accuracy of 83.8%. A risk score of
≥
2 had a sensitivity
of 85.2%, specificity of 64.9% and NPV of 86.2%. The score’s
satisfactory accuracy in predicting the diagnosis of PPCM
makes it appealing for routine use, particularly in areas where
the disease is prevalent and more expensive diagnostic facilities
are limited.
Our results have shown that in the patients, ECG
measurements were related to cardiac structure and function,
suggesting diffuse pathological changes. QRS duration modestly
correlated with LVEDD, LVESD and LVESVI, explaining 19.9%
of the variability of the latter, but had only a trend towards a
relationship with LVEF. Furthermore, QRS duration of
>
110
ms significantly increased the odds of PPCM 5.2-fold, in spite of
the faster heart rate in patients compared to controls.
These results are supported by a previous study, which
showed an association between QRS duration and mortality
among predominantly male (98%), elderly Caucasians with
moderate to severe LV systolic dysfunction caused by a variety
of diseases (LVEF
<
40%).
13
Therefore in patients presenting
with clinical features of heart failure, QRS duration
>
110 ms
could be used to suggest significant LV dilatation and systolic
dysfunction, as well as a poor prognosis.
T-wave abnormalities were identified in 68.5% of our
patients. Similar findings were reported by Ntusi
et al
. in dilated
cardiomyopathy patients, with a lower prevalence in idiopathic
(68.8%) compared to those with familial disease (87.5%), but
there was no association between such electric disturbance and
survival.
14
It seems therefore that T-wave changes, which reflect
disturbed repolarisation, may have a less detrimental effect on a
patient’s survival compared with QRS duration, which, in most,
mirrors the impact of systolic dysfunction.
In our series, QRS duration was the only ECG variable that
correlated with LV dimensions and end-systolic volume index,
while heart rate and ST–T-wave abnormalities had higher
sensitivity in predicting PPCM. Longitudinal follow-up studies
would determine the prognostic impact of ECG variables in the
setting of PPCM.
Heart rate and ST–T-wave changes seemed to independently
predict the diagnosis of PPCM. In addition, a simple score of
≥
2,
counting 1 for each of three ECG abnormalities (tachycardia,
ST–T-wave abnormalities and QRS duration
>
110 ms) had
83.8% accuracy for predicting PPCM in women at risk. These
findings could help to filter out patients requiring additional
investigations in areas with limited resources.
This study has some limitations. Firstly, serum levels of
calcium and magnesium were neither assessed nor controlled
for, but deficiencies of these electrolytes have not been reported
to be common in PPCM patients.
7
Secondly, PPCM patients
were not directly compared with patients with other conditions,
such as dilated cardiomyopathy, but we relied on published
evidence; therefore the findings cannot be considered specific to
PPCM. The sample size was small but our results are consistent
and seem to provide evidence for using easily measured ECG
variables to predict PPCM in women at risk of the disease.
Finally, echocardiography was not performed on the controls.
They were screened using clinical evaluation and ECG only,
which can be used to identify healthy women after delivery.
3
Our
findings should be considered as representative of the early stage
of the disease, while long-term electrical abnormalities remain
to be determined.
Conclusion
This study shows, for the first time, that in women presenting
within the first nine months after delivery with symptoms of
heart failure, heart rate and ST–T-wave abnormalities were
potential predictors of a diagnosis of PPCM. QRS duration
modestly correlated with LV dimensions and LVESVI. A simple
ECG-based score could potentially predict the diagnosis of
PPCM, a finding that could help to streamline the diagnosis
of PPCM prior to confirmatory investigations, particularly in
limited-resource settings, where the disease is common.
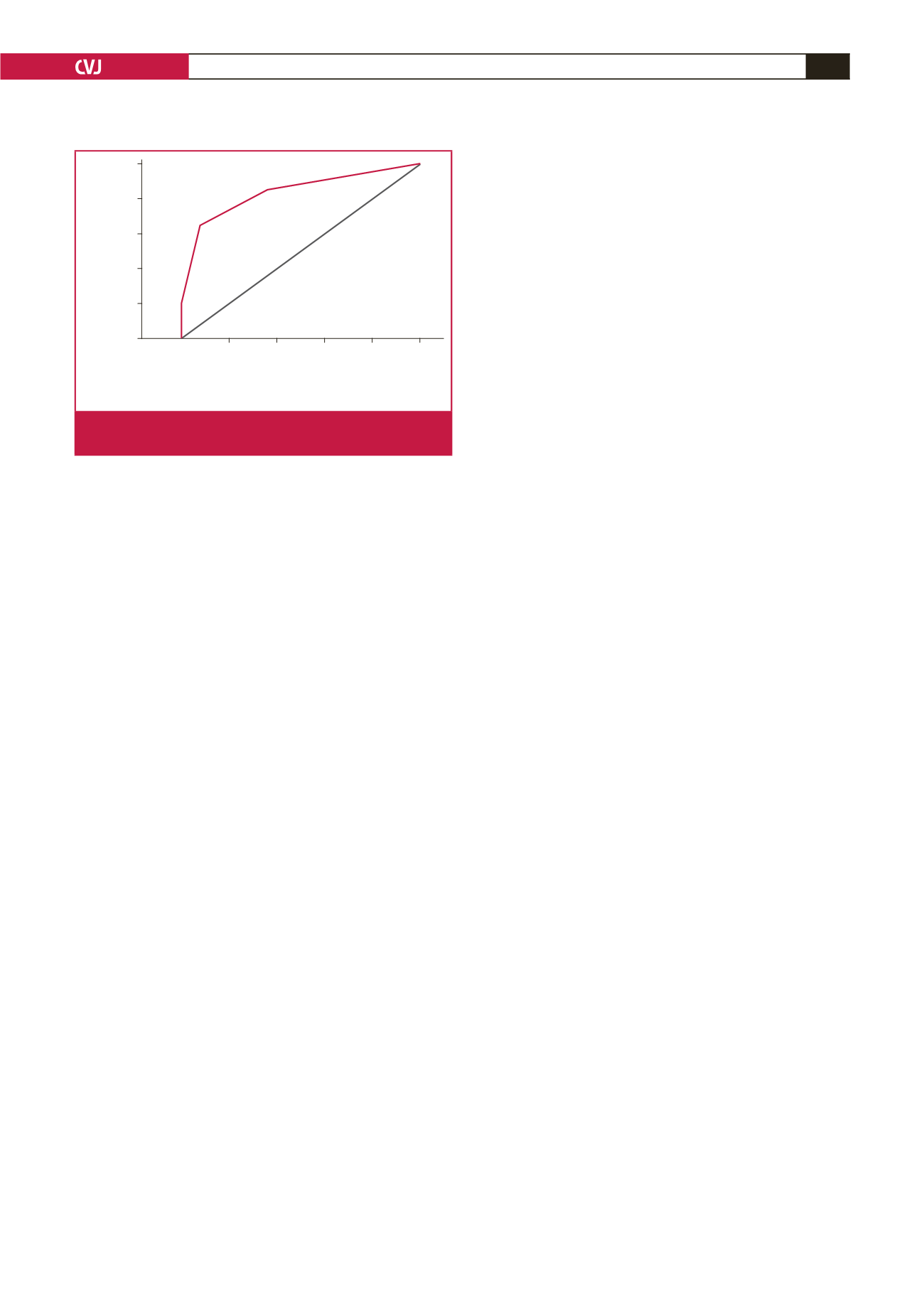
1.0
0.8
0.6
04
0.2
0.0
0.0 0.2 0.4 0.6 0.8 1.0
1 - Specificity
Sensitivity
Diagonal segments are produced by ties.
Fig. 2.
ROC curve of PPCM risk score. Area under the curve
=
83.8% (CI
=
76.4–91.18%);
p
<
0.0001.

















