
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
114
AFRICA
associated with greater risk, and a dominantly stenotic lesion
is more likely to develop complications than patients with
predominantly incompetent valves.
Prosthetic valves
Bioprosthetic valves are associated with minimal risks during
pregnancy. Conversely, mechanical valves are associated with
significant maternal and foetal complications.
36
Mechanical
prosthetic valves are exposed to two risks during pregnancy,
namely the twin risks of thrombosis and sepsis.
The procoagulant profile of pregnancy increases the
likelihood of thrombotic events, and the need to maintain
anticoagulation while protecting the foetus from exposure to
anticoagulant drugs and preventing excessive haemorrhage at
the time of delivery are contradictory therapeutic aims.
37
The use
of warfarin outside of pregnancy is both simple and cheap, with
monitoring of anticoagulant effects made easy by measurement
of the INR. In pregnancy, warfarin crosses the placenta and
leads to embryopathy, foetal anticoagulation and an increased
risk of pregnancy loss in all three trimesters. The alternative
treatment with heparin protects the foetus from direct harm
by anticoagulating only the mother; however, unfractionated
heparin is only reliably used as an intravenous infusion and the
use of LMWH requires monitoring of anti-Xa activity to know
that the patient is in the therapeutic range.
38
Notably, data from non-pregnant studies are not applicable
to pregnancy, in which the procoagulant profile changes all the
dosing schedules if a therapeutic level of anticoagulation is to
be obtained. The contradictory literature pertaining to use of
the different anticoagulants in pregnancy has been carefully
review by Elkayam with reference to the risks of both pregnancy
and the variable probability of valve thrombosis related to
the specific prosthesis and the particular valve replaced.
39
The
recommendations of these authors are contained in Table 1.
Of all the anticoagulants used, warfarin is the most effective
agent for preventing maternal valve thrombosis but also has
the highest risk of adverse pregnancy outcome. Consequently,
intensive counselling is required to explain the relative risks of
different treatment regimens and the anticipated complications
of each approach. Long-term heparin therapy is associated with
a risk of osteoporosis and heparin-induced thrombocytopenia;
these adverse effects are less frequently seen with LMWHs.
Both heparin and warfarin increase the risk of retroplacental
haemorrhage during pregnancy, and warfarin-exposed foetuses
in the first trimester risk the development of nasal hypoplasia
and epiphyseal calcification. Intravenous heparin may also
be complicated by line sepsis, which becomes a greater risk
with increasingly prolonged periods of intravenous drug
administration.
There is therefore no uniform opinion on how best to
approach anticoagulation in pregnancy. Many South African
units would use unfractionated heparin before 12 weeks of
gestation and after 36 weeks of pregnancy, in order to have
monitored control of anticoagulation that is also rapidly
reversible. Warfarin is used between these gestational ages
as a compromise that allows domiciliary care with ease of
administration and ready access to INR monitoring. There are
other ways of approaching anticoagulation, including the use
of continuous warfarin or continuous LMWH. In the latter
case, access to anti-Xa assays is necessary to ensure therapeutic
efficacy. The question of adjuvant therapy with aspirin has
been considered and certain advocates of LMWH routinely
combine aspirin with LMWH throughout pregnancy.
39
Bioprosthetic tissue valves are significantly less thrombogenic
than mechanical valves, and anticoagulation is not required,
unless associated arrhythmias are present.
36
Pregnancy may
be well tolerated in the presence of a normal valve structure,
normal left ventricular function and absence of other cardiac
lesions. Pregnancy risks increase when the valve does not
function normally. Tissue valves, however, degenerate over
time. In general, mitral bioprostheses degenerate faster than
aortic prostheses, and the rate of degeneration is more rapid
in women under 40 years of age.
40,41
Therefore, women of
childbearing age with bioprosthetic valves are likely to require
redo heart surgery, which is an important consideration when
discussing the choice of valve implant before pregnancy.
22
Sepsis is an ever-present risk in obstetric practice at the time
of delivery, although the rate of endocarditis varies widely in
the reported literature, from 0–10%.
42
The pyrexial pregnant
woman with prosthetic valves deserves careful evaluation
to exclude endocarditis as a diagnosis. The development of
endocarditis on mechanical prosthetic valves is commonly an
indication for valve replacement. The avoidance of sepsis is a
priority that requires strict protocols during and after labour.
These protocols include minimising the number of vaginal
examinations during labour, restricting instrumentation of the
genital tract during labour and delivery, scrupulous attention
to anti-sepsis during the conduct of labour, ensuring that
delivery of the placenta is complete, and the use of prophylactic
antibiotics.
Complicated disease
Pulmonary hypertension, diagnosed on the basis of estimated
pulmonary artery pressures, evident in increased peak
regurgitant velocity across the tricuspid valve, may follow
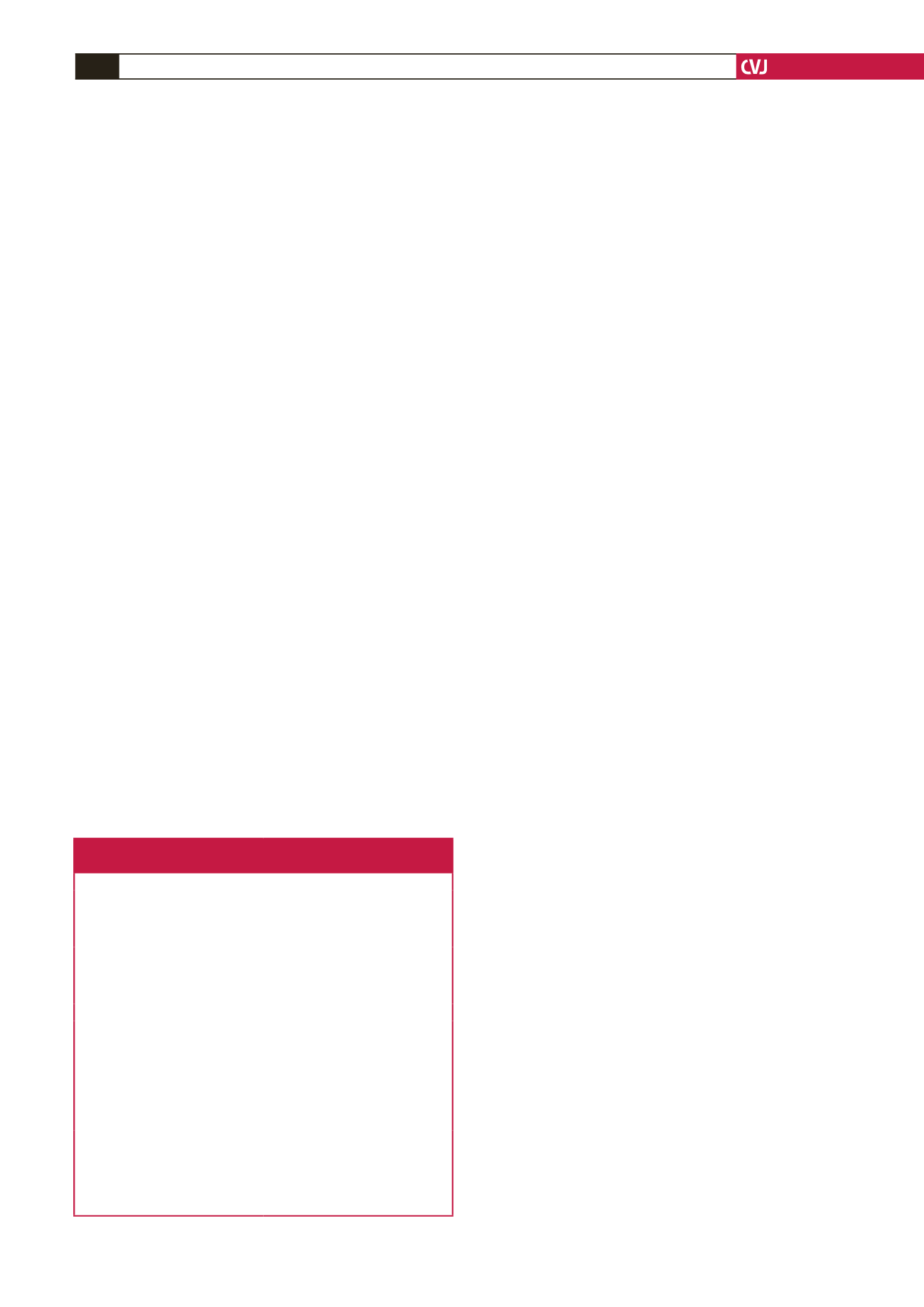
Table 1. Our recommended approach to anticoagulation therapy for
women with MPHV during pregnancy
Higher risk
Lower risk
Old-generation MPHV in mitral
position, MPHV in tricuspid posi-
tion, atrial fibrillation, history of TE
on heparin
New-generation MPHV in mitral
position and MPHV in aortic posi-
tion
Warfarin (INR 2.5–3.5) for 35 to 36
weeks followed by IV UFH (aPTT
>
2.5) to parturition
+
ASA 81–100
mg/day
LMWH SQ Q12 h (trough anti-Xa
≥
0.6 IU/ml, peak anti-Xa
<
1.5 IU/
ml) to 35 to 36 weeks, then UFH IV
(aPTT > 2.0) to parturition
OR
OR
LMWH SQ Q12 h (trough anti-Xa
≥
0.7 IU/ml, peak anti-Xa
<
1.5 IU/
ml) or UFH SQ Q12 h or IV* (mid
interval aPTT
>
2.5) for 12 weeks,
followed by warfarin (INR: 2.5–3.5)
to 35 to 36 weeks, then UFH IV
(aPTT
>
2.5) to parturition + ASA
81–100 mg/day.
LMWH SQ Q12 h (trough anti-Xa
≥
0.6 IU/ml, peak anti-Xa
<
1.5 IU/
ml) or UFH SQ Q12 h or IV* (mid
interval aPTT
>
2.0) for 12 weeks
followed by warfarin (INR: 2.5–3.0)
until 35 to 36 weeks, then UFH IV
(aPTT
>
2.0) to parturition.
*IV preferred.
aPTT = activated partial thromboplastin time; ASA = acetylsalicylic acid;
INR = international normalised ratio; IV = intravenous; LMWH = low-
molecular-weight heparin; MPHV = mechanical prosthetic heart valve; Q
= every; SQ = subcutaneous; TE = thromboembolism; UFH = unfraction-
ated heparin.

















