
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 5, September/October 2016
AFRICA
277
Methods
The study was carried out in the echocardiography laboratory
of a tertiary institution. It was a retrospective review of children
aged from birth to 17 years who were referred either by the
anaesthetist or surgeon for pre-anaesthetic echocardiographic
evaluation. Some children were referred because they had
congenital malformations for which they required surgery and
therefore needed to exclude concomitant congenital heart defects.
Others were referred for routine pre-anaesthetic cardiovascular
examination, including echo, for conditions such as oro-facial
clefts, congenital rubella syndrome and adenoidal hypertrophy.
Occasionally, some were referred by the anaesthetist or clinician
because of abnormal cardiovascular findings on clinical
evaluation. The routine cases were often referred by surgeons
while the ones with incidental findings were often referred by
anaesthetists.
The children were grouped according to the referring
departments/specialities, including restorative dentistry,
ophthalmology, ENT and other units. The other units included
paediatric surgery, and cardiothoracic and plastic surgical units.
The haematology department referred one child with sickle cell
anaemia for echo in preparation for stem cell transplantation.
This case was added to the other units.
The echocardiography register/report sheet included
information on age, gender and indication for the procedure, in
addition to the echo findings. The study period was five years,
between July 2009 and June 2014. Permission was obtained from
the institutional ethics committee to use the patients’ data.
A transthoracic echo was performed by the paediatric
cardiologist in the centre. Each child had two-dimensional,
M-mode and Doppler examinations in multiple views. Left
ventricular function was evaluated by measuring the fractional
shortening (FS) and ejection fraction (EF) with the Teichholz
method, using the Aloka Prosound SSD-4000SV (Aloka,
Meerbusch, Germany). Analysis of the reports was done
according to the recommendations of the American Society of
Echocardiography.
12
Any cardiac abnormality detected on echo
was noted. This included CHD and acquired abnormalities such
as ventricular hypertrophy and pericardial disease.
Right ventricular hypertrophy (RVH) was diagnosed when the
free wall was
>
5 mm, measured at end-diastole.
13
Left ventricular
hypertrophy (LVH) was diagnosed when the left ventricular
posterior wall was
>
13 mm, measured in systole.
14
Other
diagnoses were based on standard echo findings. The diagnosis
of CRS was made using the World Health Organisation case
definition.
15
No confirmatory laboratory tests were done because
the facilities were not available.
Statistical analysis
The data were coded and entered into IBM-SPSS version 20.1
(Chicago, IL) and analysed using the same statistical tool. The
frequencies of cardiac abnormalities are presented in simple
percentages. Continuous variables such as age are presented as
means and standard deviation (SD), or median and range if the
range of values was wide. The median values of the ages, FS
and EF between variables were compared using the Kruskal–
Wallis test. The association between variables, such as cardiac
abnormality and referring specialities, was compared using the
χ
2
test. Significance was set at
p
< 0.05 at 95% confidence level.
Results
There were 181 children recruited over the study period, of
whom 100 (55.2%) were males. The mean age was 3.0
±
3.5 years
with a range of two days to 16 years. The median age was 1.7
years.
The 181 children were referrals from dentistry (90, 49.7%),
ENT (25, 13.8%), ophthalmology (19, 10.5%) and other units
(46, 26.0%). The distribution of conditions requiring surgery for
the referred children from the various departments is shown in
Table 1.
The median ages of the cases according to the referring
department/speciality are as follows: children referred from other
units were 2.0 years (range: 2 weeks – 16 years), ENT 3.0 years
(range: 1–13 years), ophthalmology 2.0 years (range: 3 months –
11 years) and dentistry 10 months (range: 2 days – 14 years). The
difference between the median ages of patients referred by the
various specialities was statistically significant (
p
=
0.01).
Of the 181 cases referred, 39 (21.5%) had cardiac abnormalities
on echo. The abnormalities were CHD in 34 children (87.2%),
and ventricular hypertrophy in five (12.8%). The 39 children
with cardiac abnormalities consisted of 22 males (56.4%) and
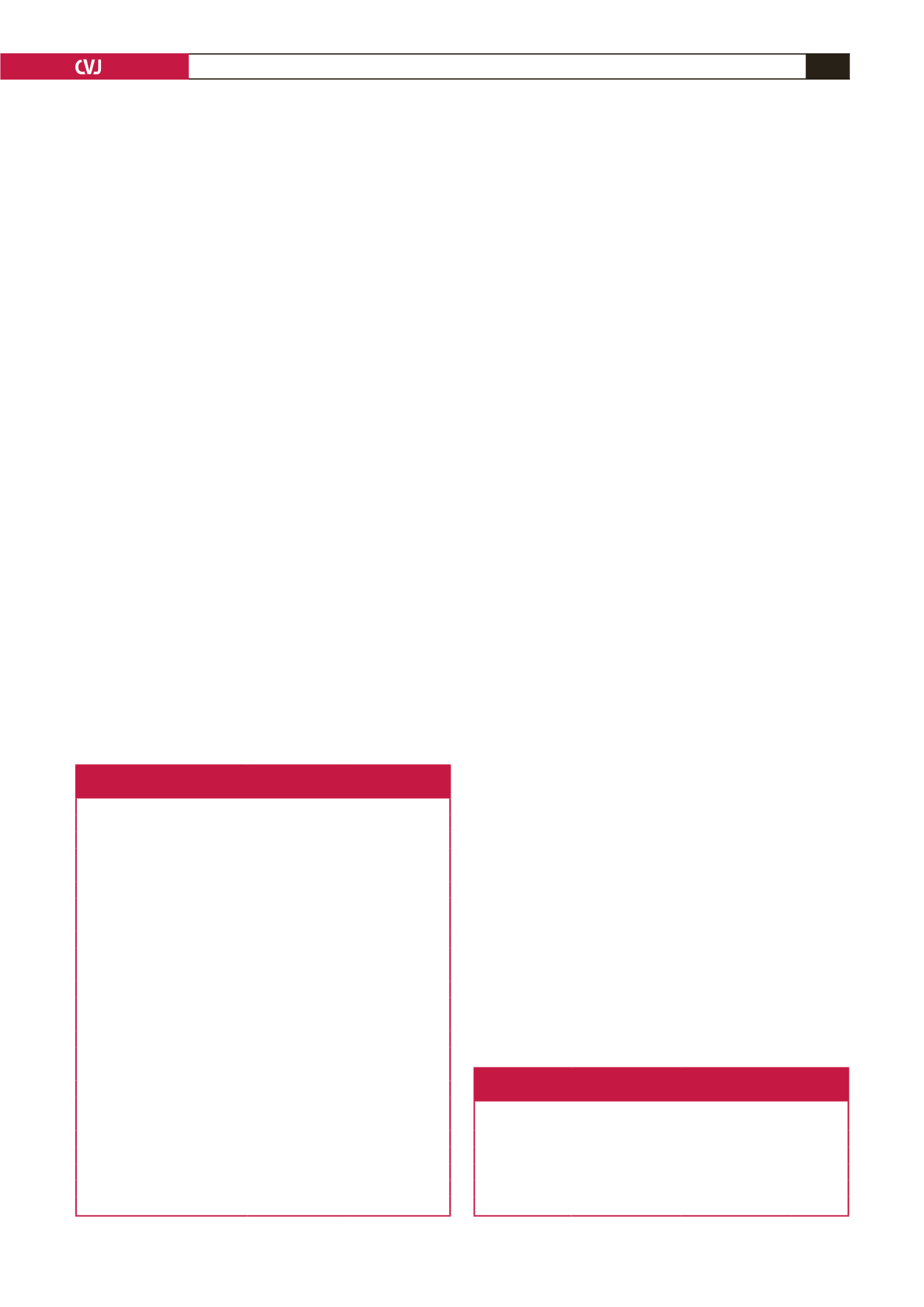
Table 1. Conditions requiring surgery referred
from the various departments
Conditions
Number
Percentage
Dentistry
Cleft lip
38
21.0
Cleft lip/palate
29
16.0
Cleft palate
20
11.1
Facial cleft
2
1.1
Paroditis
1
0.6
Ophthalmology
Cataract extraction
17
9.4
Strabismus
1
0.6
Ptosis
1
0.6
Eye agenesis
1
0.6
ENT
Adenoidectomy
23
12.7
Meamatomy
1
0.6
Mastoidectomy
1
0.6
Other units
Congenital limb abnormalities
10
5.5
Tracheo-oesophageal fistula
4
2.2
Anorectal abnormalities
3
1.7
Other congenital anomalies
11
6.1
Tumours
2
1.1
Stem cell transplantation
1
0.6
Other surgeries
15
8.3
ENT
=
ear nose and throat.
Table 2. Distribution of cases with cardiac
abnormalities by referring department
Referring speciality
Number of
cases referred
Number with
cardiac anomaly Percentage
Dentistry
90
15
16.7
ENT
25
5
20.0
Ophthalmology
20
9
45.0
Other units
46
10
21.7
ENT
=
ear nose and throat.

















