
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
AFRICA
359
of the population had no formal education, limiting their access
to quality information about healthy lifestyles. Although the
government is putting efforts into increasing awareness in these
rural and semi-urban settlements,
17,18
health education is still
largely inadequate.
Estimates from our study showed that 55.5% of the adults
had hypertension, with SDH being the commonest subtype.
This prevalence was much higher than the 29.7% reported
by Adedoyin
et al.
19
in south-western Nigeria, and the 46.4%
reported by Ejim
et al.
20
in south-eastern Nigeria. This higher
prevalence may have been related to participants being older in
our study compared to these other studies (61.6 vs 41.5 years and
61.6 vs 59.8 years, respectively).
Many studies have recorded a high prevalence of hypertension
among elderly participants. For example, Peltzer
et al.
21
in a
study among the elderly in 2008 recorded a high prevalence of
hypertension (77.3%, mean age 65 years). Other studies reported
higher prevalence rates of hypertension among older adult
population surveys in Tanzania in 2010 (69.9%, mean age 76
years), Tunisia in 2003 (69.3%, mean age 69 years) and Senegal in
2009 (65.4%, mean age 69.5 years).
22-24
Similar to Banegas
et al.
25
and Onwubere
et al.
,
26
a larger percentage of participants in our
study had ISH compared to IDH. ISH was also more common
in those above 60 years of age, compared to IDH.
Age is known to significantly influence the prevalence and
pattern of elevated blood pressure, therefore SBP tends to
increase with advancing age as a result of loss of arterial
compliance, while DBP tends to plateau or decrease after 50
years of age. The decrease in compliance results in higher SBP.
An increase in peripheral resistance is also known to result
in elevated DBP, whereas loss of elasticity in the large vessels
causes a reduction with increasing age. Therefore the net effect of
these opposing factors may results in a normal or near-normal
DBP,
27,28
depending on the predominant factor.
The prevalence of ISH obtained in this study is much
higher than in a study by Tesfaye
et al.
29
Our study showed
that only 26% of individuals with hypertension had been
diagnosed previously, 10.9% were on antihypertensive treatment,
while 22% were controlled (BP
≤
140/90 mmHg). This finding
demonstrates a high proportion of undiagnosed, untreated and
poorly controlled hypertension in Nigeria, a problem that has
been reported by others. For instance, good hypertension control
could only be achieved in 24.2% of the patients seen in a Port
Harcourt hospital.
30
Ekwunife
et al.
31
also found only 23.7 and
17.5% of males and females, respectively, with hypertension were
on antihypertensive treatment, while 5.0% of males and 17.5% of
females with hypertension were controlled.
In the present study, participants with IDH were significantly
younger than those with ISH. This is in keeping with a similar
study done by Adeoye
et al.
,
32
who found subjects with IDH to be
significantly younger among the hypertensive patients in Ibadan.
The strength of this study is in its relatively moderate sample
size that was spread across many communities. It however has
some limitations. Many of the participants were illiterate with
no recorded biodata, so the age given may not be accurate. Also,
participation in this study was voluntary, which might have
influenced the results.
Conclusion
The estimate of prevalence of hypertension obtained in this
study was higher than in most other studies in Nigeria, which
is contrary to the existing trend of low prevalence found
many years ago in semi-urban communities. The predominant
patterns of hypertension observed were both SDH and ISH.
The prevalence of hypertension was found to increase with age,
therefore age was a significant predictor of hypertension among
these subjects.
Hypertension, because of its high prevalence, deserves to be
the health priority of policy makers. Therefore policy makers
and other stakeholders in the health sector need to urgently
institute community-based strategies towards creating awareness
of hypertension, encouraging health-seeking behavioural habits,
and educating people on the main risk factors such as unhealthy
diet, high salt intake and sedentary lifestyles. It is important that
the findings of this study prompt appropriate response at state
and national levels, towards improved detection, control and
management of hypertension in Nigeria.
References
1.
Murray CJ, Lopez AD. Mortality by cause for eight regions of the
world. Global burden of disease.
Lancet
1997;
349
: 1269–1276.
2.
Cappuccio FP, Cook DG, Atkinson RW, Stuzzullo P. Prevalence, detec-
tion, and management of cardiovascular risk factors in different ethnic
groups in South London.
Health
1997;
78
: 555–563.
3.
Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, Kadiri S,
et
al
. The prevalence of hypertension in seven populations of West African
origin.
Am J Public Health
1997;
87
(2): 160–168.
4.
Olatunbuson ST, Kaufman JS, Cooper RS, Bella AF. Hypertension
in a black population: Prevalence and biosocial determinants of high
blood pressure in a group of urban Nigerians.
J Hum Hypertens
2000;
14
: 249–257.
5.
Opie LH, Seedat YK. Hypertension in sub-Saharan African popula-
tions.
Circulation
2005;
112
(23): 3562–3568.
6.
Esayas K, Yadani M, Sahilu A. Prevalence of hypertension and its risk
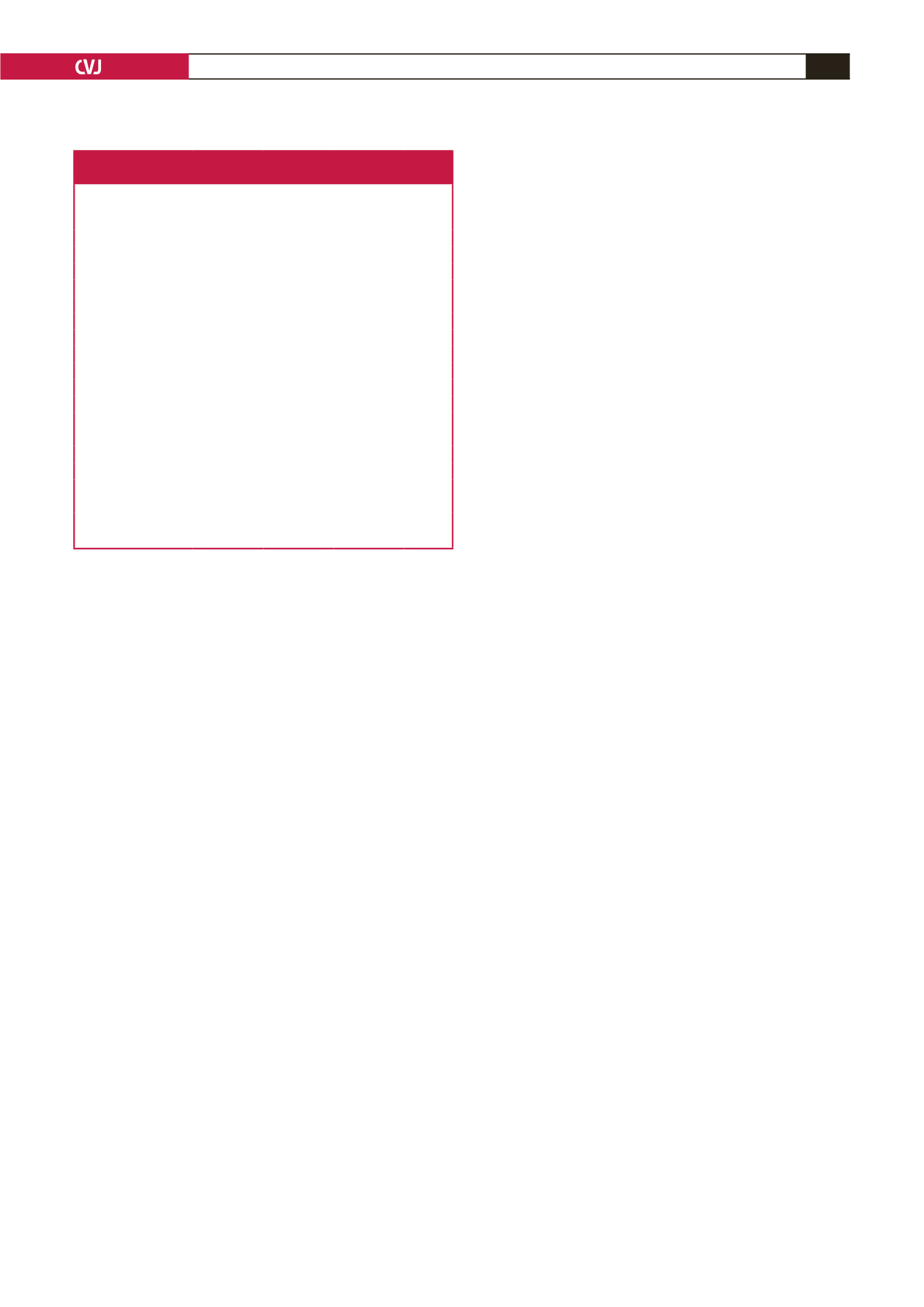
Table 3. Comparison of sociodemographic and clinical characteristics
according to hypertension subtypes
Variable
Both
(
n
=
198)
IDH
(
n
=
37)
ISH
(
n
=
181)
p
-value
Age (years)
68.2 (13.7)
61.4 (18.4)
64.4 (17.6)
0.014
Gender
Male,
n
(%)
51 (25.8)
15 (40.5)
59 (32.6)
0.117
Female,
n
(%)
147 (74.2)
22 (59.5)
122 (67.4)
Educational level
None
133 (67.2)
18 (48.6)
110 (60.8)
0.199
Primary
38 (19.2)
10 (27.0)
37 (20.4)
Secondary
17 (8.6)
4 (10.8)
24 (13.3)
Tertiary
10 (5.1)
5 (13.5)
10 (5.5)
Income (Naira)
<
20 000
174 (87.9)
29 (78.4)
151 (83.4)
0.512
20 000–40 000
18 (9.1)
7 (18.9)
21 (11.6)
41 000–60 000
4 (2.0)
1 (2.7)
6 (3.3)
61 000–100 000
1 (0.5)
0 (0.0)
3 (1.7)
>
100 000
1 (0.5)
0 (0.0)
0 (0.0)
Mean BMI (kg/m
2
)
23.4 (5.3)
24.1 (5.1)
23.7 (7.3)
0.823
Mean WC (cm)
87.3 (11.2)
88.9 (10.5)
86.5 (12.7)
0.483
Mean WHR
0.94 (0.15)
0.95 (0.05)
0.92 (0.07)
0.109
Mean SBP (mmHg)
169.8 (25.3)
125.5 (9.1)
158.3 (17.2)
<
0.001
Mean DBP (mmHg)
98.9 (9.9)
92.4 (4.4)
78.6 (7.8)
<
0.001

















