
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 3, May/June 2017
AFRICA
167
pulse pressure (37.5
±
6.9 and 38.1
±
6.3 mmHg,
p
=
0.442), and
LVEF (68.5
±
3.8 and 69.4
±
3.4%,
p
=
0.427) (Table 2).
Compared to the pre-treatment values, post-treatment
TAPSE improved (1.81
±
0.38 and 1.98
±
0.43,
p
=
0.049) (Table
2). Aortic elasticity parameters including aortic strain (15.2
±
4.8
and 18.8
±
9.5%,
p
=
0.043), aortic distensibility (7.26
±
4.71 and
9.53
±
3.50 cm
2
/dyn,
p
=
0.010) and aortic stiffness index (3.2
±
0.6 and 2.8
±
0.5,
p
=
0.045) showed significant post-treatment
improvement when compared to pre-treatment values (Table 3).
Discussion
The findings of this study demonstrate that aortic stiffness
improved after appropriate dosage medications in asthma
patients. Such improvement may be associated with the anti-
inflammatory effects of therapy. Additionally, the medication had
positive effects on right ventricular systolic functions and cardiac
output. We suggest that the decrease in aortic stiffness might have
contributed to this improvement, and we might have treated the
negative cardiac effects while treating bronchial asthma.
BA is the most common reason for paediatric respiratory
disorders and it is a significant cause of mortality and
morbidity.
1,13
Exposure to BA-associated repetitive hypoxia
results in sustained pulmonary vasoconstriction and long-term
obstruction of the pulmonary veins. In addition, pulmonary
hypertension develops, resulting in right ventricular hypertrophy
and enlargement, which is also known as cor pulmonale.
15
In our
study, the significant post-treatment increase in TAPSE can be
interpreted as improvement in right ventricular function.
The negative effects of BA on right heart functions are well
known; however, on the contrary to this well-known pathology,
there is relatively limited knowledge about how left heart
chambers are affected by this condition or how they change after
therapy. In a study assessing left ventricular function during acute
asthma exacerbations, it has been demonstrated that transmitral
peak A wave increased and E/A ratio decreased during an acute
severe asthma exacerbation, which implies the development of
left ventricular diastolic dysfunction.
16
In summary, it can be
said that both the right and the left heart functions are negatively
affected during the course of BA.
In our study, in addition to TAPSE, cardiac output and
stroke volume were significantly increased after treatment but
there was no significant difference in E/A ratio. These findings
can be interpreted as that treatment improves both right and left
heart functions. However similar E/A ratios after BA treatment
indicate that the medication had no effect on left ventricle
diastolic function. A future study designed using novel diastolic
parameters and control group could provide clearer results.
Apart from the direct impact of hypoxia on impairment
of the cardiac function and aortic stiffness in BA, some other
aetiological factors may also contribute to this situation. Indeed,
Massoud
et al
. found evidence showing the effects of chronic
and sustained inflammation on myocardial function in patients
with severe asthma. Inflammatory mediators also increase with
inflammation when the respiratory symptoms appear, and it
is known that some of these mediators have the potential to
significantly depress cardiac contractility (TNF-alpha, IL-1
β
,
IL-2, IL-6, IL-8, IL-10).
17
The patients’ symptoms recover and
the frequency of repetitions decrease with medications especially
steroids, and this might contribute to the decrease in mediator
secretion, which in turn may have resulted in an improvement of
cardiac functions and aortic stiffness at the same time.
In our study, the primary target was to evaluate the
relationship between medication and aortic stiffness and no
patient had any other chronic inflammatory disease such as
diabetes, hypertension or congestive heart failure that may have
affected aortic stiffness.
In acute severe asthma, cardiovascular function significantly
changes as a result of the direct effects of BA or secondary to
the drug therapy (
β
2
-adrenergic receptor agonists and steroids
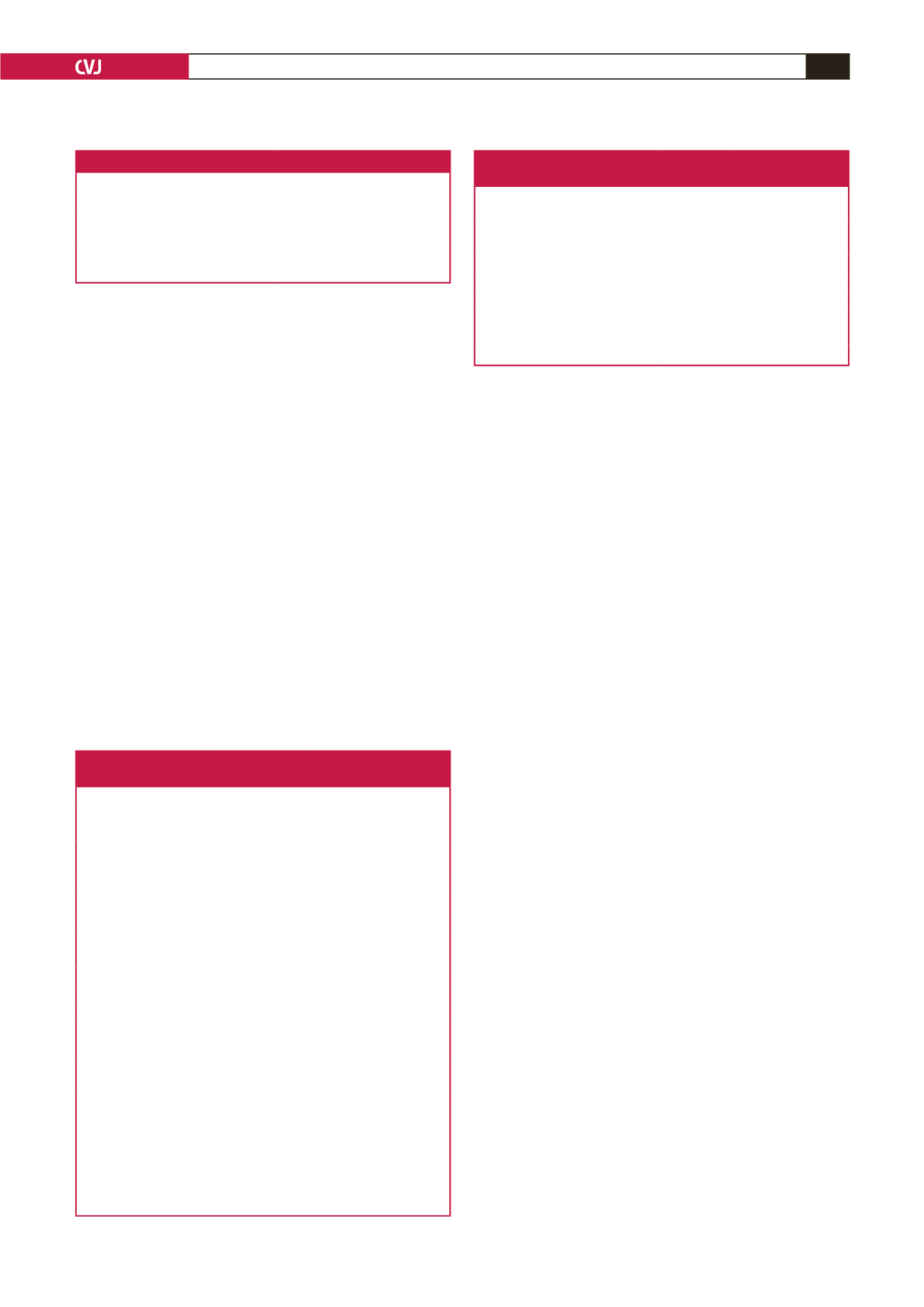
Table 1. Baseline characteristics of overall patients
Baseline characteristics
n
=
66
Mean age (years)
11.6
±
2.0
Male gender,
n
(%)
14 (56)
BMI (kg/m
2
)
17.1
±
2.5
BSA (m
2
)
1.2
±
0.5
BMI: body mass index, BSA: body surface area.
Table 2. Haemodynamic and echocardiographic findings
before and after treatment of patients
Variables
Before treatment After treatment
p-
value
HR (bpm)
90.8
±
7.7
89.5
±
7.0
0.320
SBP (mmHg)
103.8
±
10.6
102.6
±
9.0
0.280
DBP (mmHg)
65
±
7.2
66
±
8.1
0.765
Pulse pressure (mmHg)
37.5
±
6.9
38.1
±
6.3
0.442
EF (%)
68.5
±
3.8
69.4
±
3.4
0.427
LVEDV (ml)
66.2
±
13
67.9
±
15
0.124
LVESV (ml)
24.3
±
7.3
22.1
±
6.7
0.278
LVMI (g/m
2
)
55.5
±
19.4
56.2
±
18.9
0.985
IVSD (cm)
6.9
±
1.1
6.8
±
1.8
0.848
PWD (cm)
6.8
±
0.9
6.9
±
1.0
0.789
Mitral E wave (m/s)
94.0
±
14.5
95
±
15.0
0.657
Mitral A wave (m/s)
64.2
±
15.5
60.3
±
19.1
0.433
Mitral E/A
1.56
±
0.78
1.53
±
0.95
0.678
DT
134.5
±
30.7
144.7
±
41.2
0.388
TAPSE
1.81
±
0.38
1.98
±
0.43
0.049
ePASP
19.2
±
4.2
18.0
±
5.3
0.230
LA diameter (mm)
2.4
±
0.5
2.5
±
0.6
0.568
HR: heart rate, bpm: beats per minute, SPB: systolic blood pressure,
DBP: diastolic blood pressure, EF: ejection fraction, LVEDV: left
ventricular end-diastolic volume, LVESV: left ventricular end-systolic
volume, LVMI: left ventricular mass index, IVSD: interventricular
septal defect, PWD: posterior wall thickness at end-diastole, DT:
decelaration time, TAPSE: tricuspid annular plane systolic excursion,
ePASP: estimated pulmonary artery systolic pressure, LA, left atrial.
Table 3. Aortic elastic properties (strain, stiffness index,
distensibility) of patients before and after treatment
Properties
Before
treatment
After
treatment
p
-value
Aortic velocity (m/s)
0.8
±
0.1 0.9
±
0.2 0.563
Aortic diameter in systole (mm)
20.9
±
2.9 21.2
±
2.5 0.203
Aortic diameter in diastole (mm) 18.5
±
2.2 18.6
±
2.4 0.812
Aortic strain (%)
15.2
±
4.8 18.8
±
9.5 0.043
Aortic distensibility (cm
2/
dyn)
7.26
±
4.71 9.53
±
3.50 0.010
Aortic stiffness index
3.2
±
0.6 2.8
±
0.5 0.045
Cardiac output (l/min)
3.85
±
1.2 4.08
±
1.1 0.032
Stroke volume (ml)
42
±
5.0 45
±
4.2 0.044

















