
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 5, September/October 2017
AFRICA
335
on erythropoiesis-stimulating agents (ESA) versus oral iron
supplementation showed no improvement in exercise capacity
or Hb and ferritin levels with oral therapy. However in a
recent non-randomised clinical trial,
64
the researchers found that
replenishment of Hb, TSAT and ferritin produced similar results
to giving parental iron in the FAIR trial
32
in patients with HF. A
randomised trial
62
also showed ferritin and Hb levels increased
when using both parental and oral iron, although the study was
underpowered.
In a prospective study of 25 patients with cyanotic congenital
heart disease, the researchers demonstrated a significant
improvement in serum ferritin and Hb levels and the six-minute
walking test (6MWT) distance after 90 days of oral iron
supplementation with 200 mg iron fumarate three times per day.
65
The recently completed TaHeF-ID study has also shown similar
findings, with additional improvement in left ventricular ejection
fraction from 37.8 ± 12.2% to 44.5 ± 10.7% (+17%;
p
<
0.001)
and N-terminal pro B-type natriuretic peptide (NT-proBNP)
from 986 ± 774 ng/l to 582 ± 503 ng/l (–41%;
p
<
0.001) from
baseline after 90 days of a similar dosage of iron sulphate.
68
These findings are promising and justify randomised clinical
trials to address this area of uncertainty by comparing parental
and oral iron supplementation, particularly in SSA. Results from
the IRONOUT trial (NCT02188784), which is being conducted
by the National Heart, Lung, and Blood Institute’s Heart Failure
Network are also awaited.
69
Conclusions
The accumulating data on HF and anaemia/ID anaemia continue
to be largely of studies conducted in high-income countries,
with very limited information for SSA. Creating awareness and
identification of these co-morbidities in HF, both in the hospital
setting and at the population level, should be a priority. Diagnostic
dilemmas and therapeutic challenges require further exploration
in SSA, in which the pathophysiology of ID in HF and the
healthcare system may differ from that of high-income countries.
References
1.
Silverberg DS, Wexler D, Schwartz D. Is correction of iron deficiency a
new addition to the treatment of the heart failure?
Int J Mol Sci
2015;
16
: 14056–14074.
2.
Makubi A, Hage C, Lwakatare J, Mmbando B, Kisenge P, Lund LH,
et
al.
Prevalence and prognostic implications of anaemia and iron deficien-
cy in Tanzanian patients with heart failure.
Heart
2015;
101
: 592–599.
3.
Rangel I, De Sousa C. Iron deficiency status irrespective of anemia:
A predictor of unfavorable outcome in chronic heart failure patients.
Cardiology
2014;
128
: 320–326.
4.
Klip IT, Comin-Colet J, Voors AA, Ponikowski P, Enjuanes C, Banasiak
W,
et al.
Iron deficiency in chronic heart failure: An international pooled
analysis.
Am Heart J
2013;
165
: 575–582.e3.
5.
Kapoor M, Schleinitz MD, Gemignani A, Wu W-C. Outcomes of
patients with chronic heart failure and iron deficiency treated with intra-
venous iron: a meta-analysis.
Cardiovasc Hematol Disord Drug Targets
2013;
13
: 35–44.
6.
Beutler E, Waalen J. The definition of anemia: What is the lower limit
of normal of the blood hemoglobin concentration?
Blood
2006;
107
:
1747–1750.
7.
Beutler E, West C. Hematologic differences between African-Americans
and whites: the roles of iron deficiency and alpha-thalassemia on hemo-
globin levels and mean corpuscular volume.
Blood
2005;
106
: 740–745.
8.
Commentary SI, Damasceno A, Mayosi BM, Sani M, Ogah OS, Mondo
C,
et al.
The causes, treatment, and outcome of acute heart failure in
1006 Africans from 9 countries.
Arch Intern Med
2012;
172
: 1386–1394.
9.
Ogah OS, Stewart S, Falase AO, Akinyemi JO, Adegbite GD, Alabi AA,
et al.
Contemporary profile of acute heart failure in Southern Nigeria:
data from the Abeokuta Heart Failure Clinical Registry.
JACC Heart
Fail
2014;
2
: 250–259.
10. Stewart S, Wilkinson D, Hansen C, Vaghela V, Mvungi R, McMurray
J,
et al.
Predominance of heart failure in the Heart of Soweto study
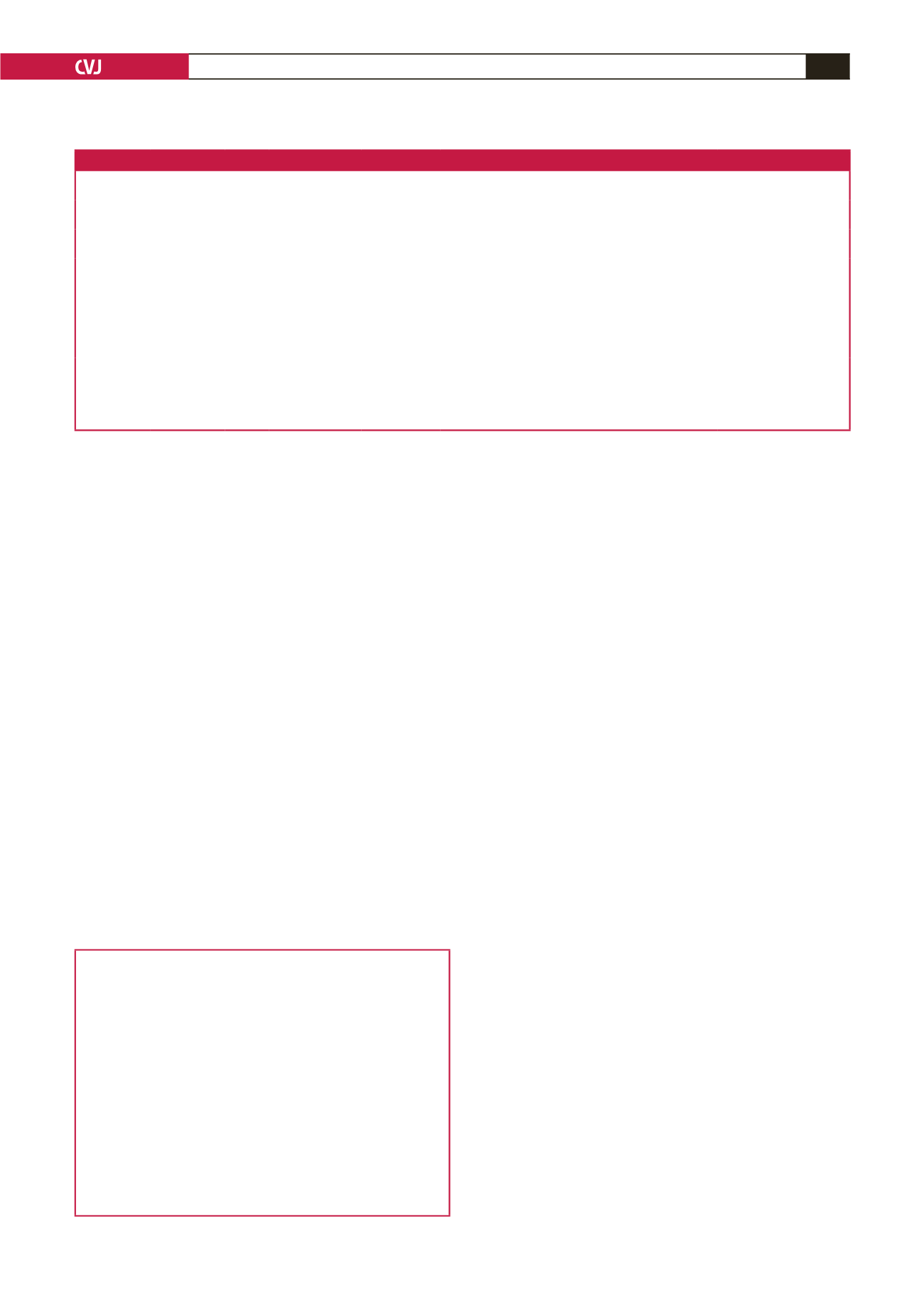
Table 6. Study reporting oral iron therapy as an interventional drug or placebo in HF
Author, year
Study design
Sample
size
Type of iv iron
Dose
Target
dose
Benefits
Adverse effect/toxicity
Niehau
et al
.
64
2015
Observational
105 Oral iron (NS)
NS, 180 days
Iron
repletion
↑
Hb,
↑
SF,
↑
TSAT,
↑
Iron,
↑
TIBC
NR
Tay
et al
.
65
2010
Observational
25 Ferrous fumarate 200 mg 3×/day,
12 weeks
Iron
repletion
Hb, ferritin, TSAT, 6MWT
No adverse effect
Beck-da-Silva
et al
.
62
2013
Controlled 18 Ferrous sulphate 200 mg 3×/day,
8 weeks
NR
↑
Hb,
↑
Ferritin,
↑
TSAT,
↑
peak VO
2
,
↑
NHYA
NR
Parissis
et al
.
66
2008
Controlled 24 Ferrous sulphate 250 mg twice a
day, 12 weeks
NR No change in QoL, Hb, significant deteriora-
tion in exercise capacity
1 TIA, 1 constipation
Van Velduisen
et al
.
63
2007
Controlled 165
Oral iron
200 mg/day,
26 weeks
NR No change in exercise capacity, Hb, ferritin,
TSAT, minor improvement in QoL, NYHA
class
Adverse effect comparable
to ESA including discon-
tinuation, HF, HT, DVT
Palazzuoli
et
al
.
67
2006
Controlled 40 Ferrous gluconate 300 mg/day
12 weeks
NR No changes in NYHA, exercise capacity, Hb,
BNP, creatinine
NR
iv: intravenous, NS: not specified, NR: not reported, Hb: haemoglobin, SF: serum ferritin, TSAT: transferrin saturation, NYHA: New York Heart Association,
6MWD: six-minute walking distance, VO
2
: oxygen consumption, QoL: quality of life, TIBC: total iron-binding capacity, TIA: transient ischaemic attack, ESA: erythro-
poiesis stimulating agent, DVT: deep-vein thrombosis, HT: hypertension, BNP: B-type natriuretic peptide.
Key points
•
Anaemia and ID are both common in HF and have
prognostic implications
•
In both conditions, the epidemiology, diagnosis and
therapies have been extensively studied in developed
countries but are largely unexplored in SSA
•
Studies are needed to provide more insight into the
burden and peculiarities of and intervention for anaemia
and ID in HF in SSA, in which the pathophysiology may
be different from that in high-income countries.
•
Although intravenous iron supplementation appears
to be beneficial in the treatment of patients with HF
and ID, oral iron supplementation may be a potential
alternative in resource-limited countries such as in SSA.

















