
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 5, September/October 2018
AFRICA
291
trimester, she had required treatment for infective endocarditis,
complicated by acute kidney injury and disseminated intravascular
coagulation. She was discharged after this episode and readmitted
a week later at 36 weeks, as per protocol. Normal vaginal delivery
followed and she was discharged six days later in a satisfactory
condition. She returned to casualty 41 days post-delivery and
complained to the prehospital crew that she was unable to hear
her valve clicks. Her INR was 3.73 (supra-therapeutic). She then
suffered a cardiorespiratory arrest and could not be resuscitated.
The cause of death was unclear, however it was suspected
to be a valve thrombosis on the basis that she complained that
she was unable to hear her valve clicks. She had had no INR
monitoring between discharge post-partum and her presentation
in cardiac arrest.
The second death occurred in a 36-year-old patient with a
double valve replacement (mitral and aortic) necessitated by
Takayasu’s disease. She had tight aortic stenosis with pulmonary
hypertension using standard criteria and was assessed as high
risk for surgical revision, although this was considered ‘semi-
urgent’. There was extensive vascular involvement, including
total occlusion of the left carotid and of both subclavian vessels
as well as severe stenosis of other head and neck vessels. She was
also HIV infected (CD4 count was 321 cells per mm
3
) and had
defaulted on antiretroviral therapy. This was restarted late in
pregnancy. Additionally, she was rhesus negative. There was also
a history of previous tuberculosis, which had been fully treated.
Due to the very high-risk nature of the pregnancy, the patient
was offered a termination of pregnancy, which she declined.
At 31 weeks’ gestation, she had spontaneous rupture of the
membranes and two days thereafter required a caesarean section.
She was discharged seven days postpartum but represented
two days later requiring intubation for pneumonia and ICU
admission. Her clinical course was complicated by acute kidney
injury, supraventricular tachycardia requiring cardioversion,
pneumonia and a brainstem infarct. Intensive care was
subsequently withdrawn and the patient died.
There were three cases of stroke and one patient with a clot
on a prosthetic valve. One HIV-negative patient developed a left
middle cerebral artery infarct while on a heparin infusion at nine
weeks’ gestation, presumably after a thrombotic event. At the
time, her PTT was 2.4 times that of the control. Despite the risks
of warfarin in the first trimester, she was changed to warfarin-
based anticoagulation after this event.
A second patient developed a brainstem infarct post-partum
while intubated. On the four days preceding confirmation of
the infarct on CT brain scan, her INR measurements ranged
between 2.8 and 6.04. This patient, who died following her
infarct and is described in more detail above, had multiple risk
factors for stroke, including Takayasu’s arteritis and HIV.
A third patient developed an ischaemic stroke in the first
trimester, prior to diagnosis of pregnancy. At the time, her INR
was 1.35. The stroke resulted in right hemiplegia and aphasia.
This patient was also HIV positive and attended the maternity
clinic for the first time in the third trimester. The aetiology of
the stroke remains unclear and may not have been embolic or
thrombotic in nature, but rather an ischaemic stroke due to HIV
infection.
A fourth, HIV-negative patient, was noted to have a ‘small clot
on her valve’ at routine echo while receiving a sub-therapeutic
dose of heparin. This resulted in no adverse sequelae. The first
death, described above, may have been due to a valve thrombosis
but this was unproven. No deep-vein thromboses or pulmonary
emboli were detected.
Major haemorrhage occurred in six pregnancies (Table 4).
These included four major haemorrhages in term deliveries and
two major haemorrhages in pregnancies terminating at 11 and
19 weeks, respectively.
Of the four term deliveries, there were two episodes of
haemorrhage related to sepsis and two wound haematomas
requiring return to theatre. Sepsis contributed to two major
haemorrhages. One patient with puerperal sepsis, who delivered
by caesarean section, needed total abdominal hysterectomy and
bilateral salpingo-oophorectomy as well as massive transfusion
for post-operative bleeding. Another patient with puerperal sepsis
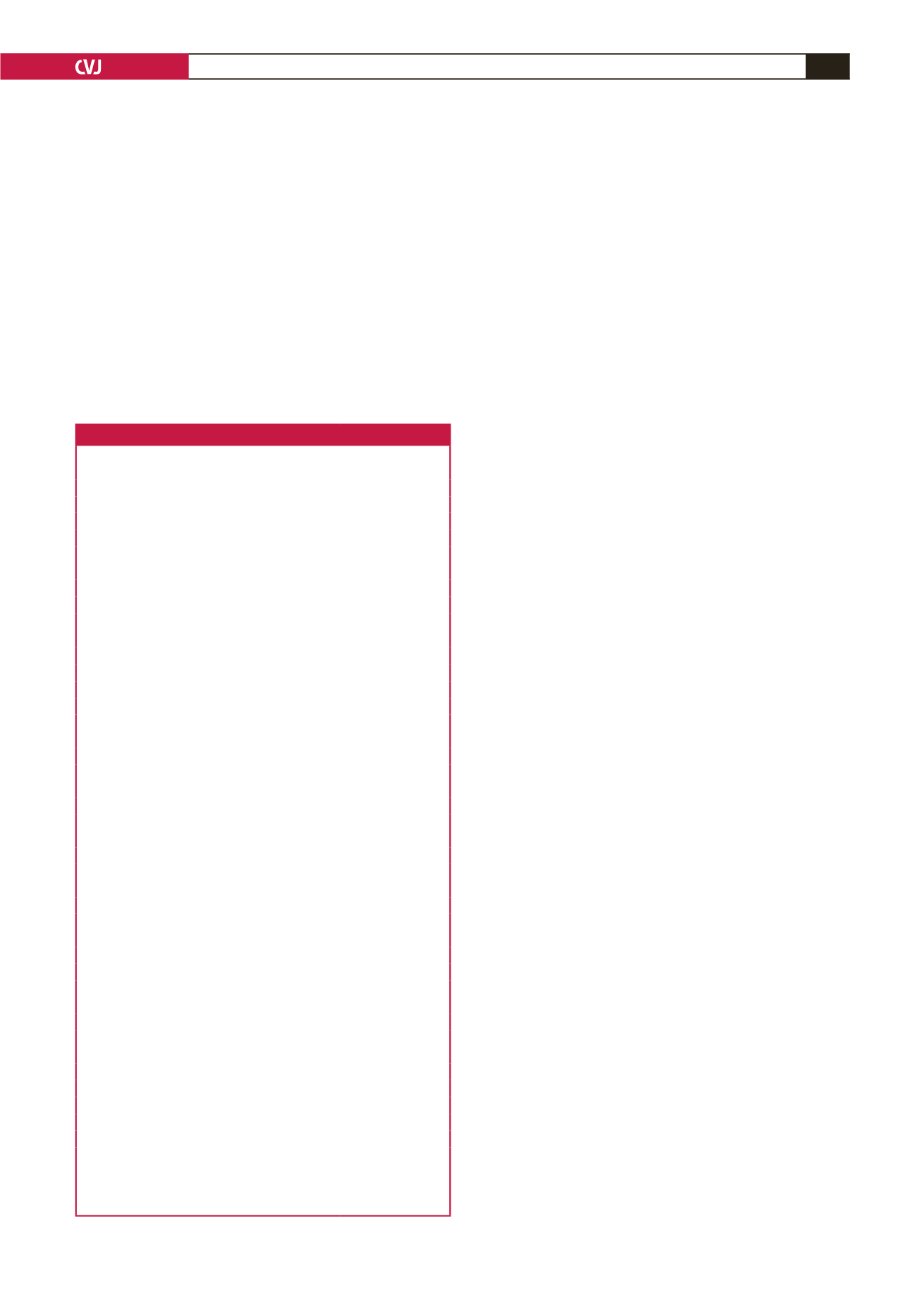
Table 3. Baseline maternal characteristics (
n
=
29)
Characteristics
Mean
±
SD or
n
(%)
Age at delivery (years)
27.9
±
7.9
Weight (kg) (
n
=
26)
70.2
±
13.8
NYHA FC,
n
(%)
I/II
29 (100)
III
0 (0)
Vital signs
Heart rate (bpm)
90
±
18
SBP (mmHg)
111
±
16
DBP (mmHg)
72
±
11
Echocardiogram (
n
=
25)
LVEDD (mm)
50.1
±
9
LVESD (mm)
35.8
±
9.8
EF (%)
54.4
±
13.7
ECG (
n
=
27),
n
(%)
Sinus rhythm
22 (81)
Atrial fibrillation
5 (19)
Atrial flutter
1 (4)
RBBB
1 (4)
Medical history
HIV
10 (34)
Syphilis
2 (7)
Other (psoriasis, hearing impairment)
2 (7)
Reason for valve replacement,
n
(%)
Rheumatic heart disease
22 (97)
Takayasu’s
1 (3)
Position of valves,
n
(%)
Mitral
18 (62)
Aortic
3 (10)
Mitral and aortic
8 (28)
Warfarin dose,
n
(%)
≤ 35 mg/week
10 (35)
>
35 mg/week
14 (48)
Undocumented
5 (17)
Obstetric history,
n
(%)
Primigravida
6 (21)
Multigravida
23 (79)
Gestation age at presentation,
n
(%)
<
6 weeks
2 (7)
<
12 weeks
14 (48)
12–24 weeks
8 (28)
≥
24 weeks
5 (17)
kg: kilogram, NYHA FC: New York Heart Association functional class, bpm:
beats per minute, SBP: systolic blood pressure, DBP: diastolic blood pressure,
LVESD: left ventricular end-systolic diameter, LVEDD: left ventricular end-
diastolic diameter, EF: ejection fraction, ECG: echocardiogram, RBBB: right
bundle branch block.

















