CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 1, January/February 2019
48
AFRICA
stenting (stenting after thrombus aspiration without balloon
pre-dilatation) was performed in 51.9% of the patients with
IC administration and in 53.7% of those treated with IV
administration (
p
=
0.851).
Angiographic outcome is presented inTable 4. Post-procedural
TIMI flow grade was similar in both groups, with achievement
of a TIMI 3 flow grade in 89.7% of patients with IC and in 89%
of those with IV administration (
p
=
0.747). Post-procedural
MBG 3 was obtained in 62.8% of patients with IC and in 63.4%
of those with IV administration (
p
=
0.235). An MBG
≥
2 was
more frequently obtained with IC versus IV administration
(89.7 vs 81.7%), but this did not reach statistical significance (
p
=
0.148).
There was no difference between patients randomised to IC
and IV abciximab with regard to ST-segment resolution rate.
ST-segment resolution
≥
70% was achieved in 36 of 78 patients
with IC versus 30 of 82 patients with IV abciximab bolus (46.1
vs 36.6%,
p
=
0.368). Partial ST-segment resolution was achieved
in 28 of 78 versus 31 of 82 patients (35.9 vs 37.8%,
p
=
0.368).
No resolution was observed in 14 of 78 versus 21 of 82 patients
(17.9 vs 25.6%,
p
=
0.368) with IC and IV abciximab bolus,
respectively.
In-hospital outcome: major cardiac events are listed in Table
5. Occurrence of death, recurrent myocardial infarction and
target revascularisation rates within 30 days were similar in the
two groups. There were three deaths in each group (mortality
rate: 3.8%). MACE occurred in six of 78 patients given the IC,
and seven of 82 patients given the IV abciximab bolus (7.6 vs
8.5%,
p
=
0.410). One stroke occurred in each group, and two
patients in the IC and nine in the IV group developed renal
failure (2.5 vs 10.9 %,
p
=
0.414).
Major bleeding complications occurred in one patient in
the IC group and none in the IV group. Minor bleeding
complications occurred in seven of 78 patients given IC versus
eight of 82 patients given the IV abciximab bolus (9.3 vs 9.9%,
p
=
0.578). Thrombocytopenia occurred in five of 78 patients with
IC versus three of 82 patients with IV abciximab (6.4 vs 3.7%,
p
=
0.414).
Short-term clinical outcome: after the one-month follow
up, there was only one cardiac death in each group, one stent
thrombosis in the IC group, and similar rates of MACE in both
groups (2.66 vs 2.53%,
p
=
0.588). Also, there was no difference
in mortality rate (one death in the IV group), stent thrombosis
(one in the IC group) and MACE (5.9 vs 8.8%,
p
=
0.714) after
six months of follow up.
Discussion
This study was intended to assess the potential benefit of IC over
IV abciximab administration after manual thrombus aspiration
in patients undergoing primary PCI for STEMI. It showed that
distal, intralesional IC administration of abciximab through the
aspiration catheter following aspiration thrombectomy did not
provide additional benefit over IV administration of the drug.
Among 160 patients randomised to either IC or IV
abciximab bolus, no significant difference between the two
groups was observed. Baseline clinical characteristics of patients,
symptom-to-balloon time, which impacts on MBG,
25
coronary
angiography findings, infarct-related coronary artery, target
vessel and procedural characteristics were similar in the two
groups. Reperfusion parameters including the primary outcome
endpoint, ST-segment resolution, and the secondary endpoint,
achievement of MBG grade
≥
2, did not differ between the
groups. Also, no difference was observed with regard to the rate
of MACE and major bleeding.
Over the past decade, several approaches have been used to
prevent or reverse the no-reflow phenomenon. This included
aspiration thrombectomy and intralesional administration of
glycoprotein IIb/IIIa inhibitors via dedicated perfusion catheters
to achieve higher concentration of the drug at the coronary
vascular bed in order to improve myocardial reperfusion and to
reduce infarct size.
Initial results from the Thrombus Aspiration during
Percutaneous Coronary Intervention in Acute Myocardial
Infarction (TAPAS) trial suggested that aspiration
thrombectomy could be effective in improving revascularisation
at the microvascular level.
7
Also, a meta-analysis of randomised
trials, including 3 996 patients, showed improved myocardial
perfusion, as assessed by ST-segment resolution and MBG.
8
However, aspiration thrombectomy was subsequently challenged
by the results of two trials, Thrombus Aspiration in ST-elevation
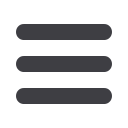
Table 3. Procedural characteristics
Variables
All
patients,
n
=
160
IV abcix-
imab,
n
=
82
IC abcix-
imab,
n
=
78
p
-value
Radial access,
n
(%)
116 (72.5) 57 (69.5) 59 (75.6) 0.385
Aspiration thrombectomy,
n
(%) 130 (81.3) 68 (82.9) 62 (79.5) 0.577
Predilatation,
n
(%)
49 (30.6) 29 (35.4) 20 (25.6) 0.182
Direct stenting,
n
(%)
83 (51.9) 44 (53.7) 39 (50)
Delayed stenting,
n
(%)
58 (36.3) 28 (34.1) 30 (38.5) 0.851
UFH 5 000 IU,
n
(%)
135 (84.4) 75 (91.5) 60 (76.9) 0.011
UFH 2 500 IU,
n
(%)
25 (15.6)
7 (8.5)
18 (23.1)
Clopidogrel 300 mg,
n
(%)
13 (18.1)
6 (7.3)
7 (9)
Clopidogrel 600 mg,
n
(%)
147 (91.9) 76 (92.7) 71 (91)
0.701
Abciximab IV perfusion,
n
(%)
112 (70)
64 (78)
48 (61.5) 0.074
UFH: unfractioned heparin.
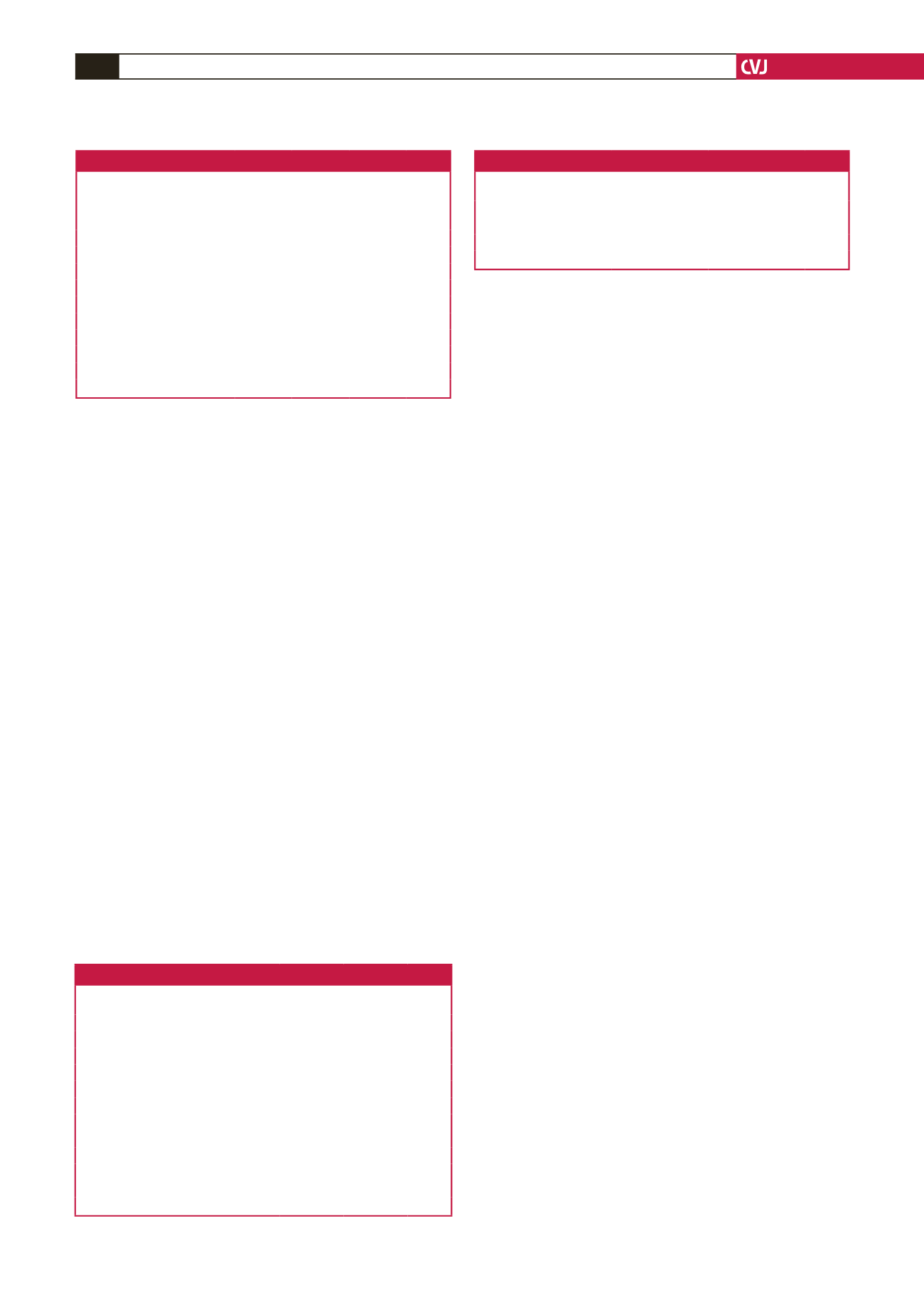
Table 4. Angiographic outcomes
Variables
All patients,
n
=
160
IV abcix-
imab,
n
=
82
IC abcix-
imab,
n
=
78
p
-value
Post-procedural TIMI flow:
0,
n
(%)
3 (1.9)
1 (1.2)
2 (2.6)
0.747
2,
n
(%)
14 (8.8)
8 (9 .8)
6 (7.7)
3,
n
(%)
143 (89.4)
73 (89)
70 (89.7)
Post-procedural MBG:
0,
n
(%)
8 (5)
4 (4.9)
4 (5.1)
1,
n
(%)
15 (9.4)
11 (13.4)
4 (5.1)
0.235
2,
n
(%)
36 (22.5)
15 (18.3)
21 (26.9)
3,
n
(%)
101 (63.1)
52 (63.4)
49 (62.8)
MBG 0/1,
n
(%)
23 (14.4
15 (18.3)
8 (10.3)
MBG 2/3,
n
(%)
137 (85.6)
67 (81.7)
70 (89.7)
0.148
TIMI: thrombolysis in myocardial infarction; MBG: myocardial blush grade.
Table 5. Major cardiac events
Events
IV abciximab,
n
=
82
IC abciximab,
n
=
78
p
-value
Heart failure,
n
(%)
4 (4.9)
3 (3.8)
Cardiac death,
n
(%)
2 (2.4)
3 (3.8)
0.414
Non-cardiac death,
n
(%)
1 (1.2)
0 (0)
Major cardiac events,
n
(%)
7 (8.5)
6 (7.6)

















