
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 3, May/June 2019
AFRICA
163
PCI performed more than 24 hours after admission. STEMI
was defined as follows: ST-segment elevation consistent with
a myocardial infarction (MI) of at least 2 mm in contiguous
precordial leads and/or ST-segment elevation of at least 1 mm in
two or more limb leads or new left bundle branch block; positive
cardiac necrosis markers (CK-MB and/or troponin T).
The baseline and post-procedural blood flow in the IRA
was quantified with the TIMI grading system.
15
Slow flow was
defined as a decrease in TIMI flow from 3 to 2 during the
procedure; no re-flow was defined as decrease in TIMI flow from
3 or 2 to either 0 or 1 during the procedure.
16
After the diagnosis of STEMI was confirmed, all patients
received clopidogrel (300 mg loading dose followed by 75 mg
orally once daily) and aspirin (300 mg loading dose followed by
100 mg orally once daily). Statins, angiotensin converting enzyme
(ACE) inhibitors/angiotensin receptor blockers (ARBs) and
beta-blockers were routinely prescribed if no contra-indications
existed. Low-molecular-weight heparin (LMWH) was instituted
according to current guideline recommendations. A glycoprotein
(GP) IIb/IIIa receptor antagonist was administered based on the
decision of the operator.
At the time of diagnostic angiography, epicardial blood flow
was assessed via the TIMI grading system. All angiograms were
reviewed by two experienced operators who were blinded to all
data apart from the coronary angiograms.
The primary endpoint was procedural success, defined as
a final diameter stenosis of less than 30%, TIMI 3 flow, no
occurrence of slow flow, and no re-flow or distal embolisation.
The secondary objectives were in-hospital mortality and major
adverse cardiac events (MACE), defined as heart failure, recurrent
angina pectoris, target vessel revascularisation or arrhythmia.
It is routine in our hospital, after discharge, for out-patient
nurses to record information of STEMI patients’ adherence
to medication, tolerance of activity and well-being every three
months. We collected all the information needed for one year of
follow up, according to out-patient records. Re-hospitalisation
due to heart failure, recurrent angina pectoris, target-vessel
revascularisation or arrhythmia were regarded as MACE.
Statistical analysis
Statistical analysis was conducted with Statistical Package for
the Social Sciences (SPSS) 17.0 software (SPSS Inc, Chicago,
IL, USA). Numerical variables are represented as the mean
±
standard deviation or median, and categorical variables as
percentages or rates. To test differences between the groups, the
Student’s
t
-test was used for numerical variables with a regular
distribution, and the Mann–Whitney
U
-test was employed if
there was an irregular distribution. Categorical variables were
analysed with the chi-squared and Fisher’s exact tests. Kaplan–
Meier survival analysis was used for the analysis of endpoints
that occurred after the follow-up period, and a log rank test
was performed to test the differences. A
p-
value of
<
0.05 was
regarded as statistically significant.
Results
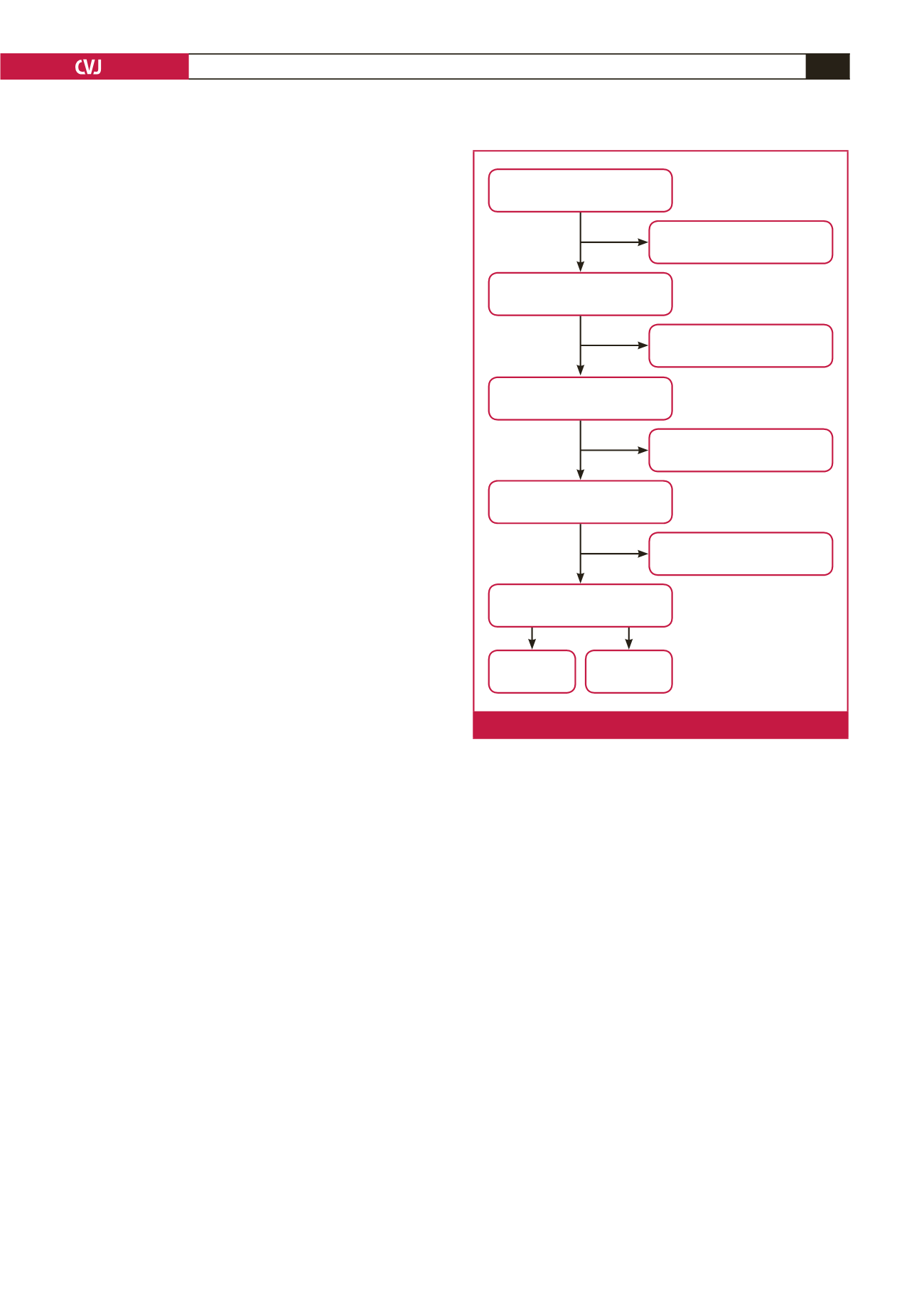
From 1 January 2008 to 1 January 2015, a total of 729 STEMI
patients who presented late after onset of symptoms were
admitted to our department; 251 of the 729 patients presented
with an IRA TIMI flow of grade 0 to 1, and 228 patients
presented after 72 hours of symptom onset. Of the remaining
250 patients, PCI was not performed in 85 patients. Six were
also excluded because they exhibited cardiac shock or electrical
instability. Finally, 159 patients were included in the study.
Emergency PCI was performed in 73 patients and delayed
PCI in 86 patients (Fig. 1). The average age was 63 years and
78% were male. There were no significant differences between
the two groups in terms of baseline clinical characteristics except
that patients in the delayed PCI group had higher high-sensitivity
C-reactive protein (hs-CRP) and elevated fasting glucose levels.
The time from symptom onset to admission or PCI was shorter
in the emergency PCI group compared with the delayed PCI
group (Table 1).
As shown in Table 2, there were more patients whose most
recent chest pain occurred within 12 hours before admission
in the emergency PCI group compared with the delayed PCI
group (36.9 vs 18.6%,
p
=
0.012). Loading doses of aspirin and
clopidogrel were given in both groups of patients, as described
in the study protocol. Dual antiplatelet therapy (more than one
day) and LMWH pre-PCI were administered more often in
the delayed group compared with the emergency group (94.2
vs
10.8%,
p
<
0.001; 94.2 vs 0%,
p
<
0.001; 100
vs
8.5%,
p
<
0.001), and the emergency group had a higher rate of GPIIb/IIIa
receptor antagonist use during the procedure (24.3%) compared
with the delayed PCI group (4.7%,
p
=
0.015).
1 Jan 2008 to 1 Jan 2015
729 STEMI patients present late
478 patients present > 12 hours
with IRA TIMI 2–3
250 patients present
12–72 hours, IRA TIMI 2–3
165 patients present 12–72 hours, IRA
TIMI 2–3 and PCI were performed
159 patients present 12–72 hours, IRA
TIMI 2–3 and PCI was performed and stable
Emergency
group (
n
= 73)
Delayed group
(
n
= 86)
251 patients, IRA TIMI 0–1
228 patients present > 72 hours
No PCI in 85 patients
6 patients with cardiac shock or
electrical instability
Fig. 1.
Selection of patients for the study.

















