
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 3, May/June 2019
AFRICA
e5
found in the left atrium, attached to the inter-atrial septum.
The myxoma was removed with approximately 1 cm of the
inter-atrial septum. After the cardiac chambers were inspected
and no additional tumours were found, the atrial septal defect
was repaired with a bovine pericardial patch. The duration of
cardiopulmonary bypass was 70 minutes and aortic clamp time
was 45 minutes.
The postoperative course of both patients was uneventful.
Histological examination of the masses confirmed myxoma.
Postoperative echocardiographic examination showed no
abnormalities. Because the mother had postoperative wound
infection in the femoral incision and the daughter had had a
medical abortion before the operation, they were both discharged
after about 15 days.
Discussion
Carney complex, which is a syndrome of cardiac myxomas,
spotty pigmentation (lentiginosis) and endocrine overactivity,
was first described in 1985 by J Aidan Carney.
3
It comprises 7%
of all cardiac myxomas and can be found in all ages, especially
young women.
A diagnosis of Carney complex is made based on a detailed
patient history, thorough clinical evaluation, a variety of
specialised tests and identification of the chracteristic symptoms.
To make a diagnosis of Carney complex, patients must have
two major criteria (cardiac myxoma, skin myxoma, lentiginosis,
acromegaly, testicular tumour, thyroid tumour or other endocrine
tumours) or one major plus one supplemental criteria [affected
first-degree relative, activating mutation of protein kinase
cAMP-activated catalytic subunit-alpha (PRKACA) and protein
kinase cAMP-activated catalytic subunit-beta (PRKACB) or
inactivating mutation of protein kinase type I-alpha regulatory
subunit (PRKAR1A) gene]
4
(Table 1).
These cases were similiar to Carney complex; they had
cardiac myxoma and lentiginosis. The recurrence interval was
four years for both mother and daughter. They each had three
cardiac operations for left atrial myxomas at the same time
periods. We did not have any genetic or hormonal analysis done.
Cardiac myxomas related to Carney complex more frequently
occur in the left ventricle, compared with sporadic myxomas.
Edwards
et al
. reported that 64% of cardiac myxomas related
to Carney complex occurred in the left atrium, 44% in the right
atrium, 14% in the left ventricle and 12% in the right ventricle.
5
In our cases, the myxomas appeared in the left atrium.
Myxomas usually show signs of obstructed ventricular
filling, thereby mimicking a mitral or tricuspid valve stenosis.
Production and release of interleukin 6 by the tumour cells gives
rise to non-specific symptoms such as fatigue, weight loss, fever
and arthralgia. The symptomatology in recurrent myxomas is
the same as in general non-recurrent myxomas.
6
These patients
had constitutional symptoms at each recurrence; the daughter
also had symptoms mimicking mitral valve stenosis.
Gerbode
et al
. encountered the first recurrence of a myxoma
after removal.
7
The mechanism of recurrence can be explained
by incomplete resection of the original tumour, leading to
regrowth; familial predisposition for recurrence; intra-cardiac
tumour seeding of the first one; and due to the existence of a
pre-tumoural focus in the myocardium, leading to recurrence.
6
In these two cases, the reason was most probably due to family
predisposition.
Predicting recurrence of cardiac myxomas is still an open
question. Keeling
et al
. found significant immunological changes
in myxoma patients. In the case of recurrence, serum protein
electrophoresis, C-reactive protein, fluorescense-activated cell
sorter, interleukin 2 receptor and intracellular adhesion molecule
levels may be altered. Immunological and genetic screening of
these patients may help to identify patients at risk for additional
recurrence.
8
Normally, echocardiographic follow up should be
performed each year to detect myxoma recurrences early. Patients
with known Carney complex should have this examination every
six months if they have already had a surgical resection.
9
Myxomas usually appear as well-defined, smooth, oval or
lobular lesions that are commonly pedunculated. Normal intra-
cardiac structures and embryological remnants can sometimes
be mistaken for atrial myxomas on TTE. Transoesophageal
echocardiography (TEE) may demonstrate the site of
insertion and other surface features of the myxoma, as well
as haemorrahage, necrosis, cysts and calcification. TEE has
limitations in viewing the right heart and extra-cardiac structures,
and requires sedation.
Cardiac magnetic resonance imaging has become increasingly
valuable for determing cardiac tumours. It is very useful to
differentiate myxomas from other cardiac masses, thrombus
and anatomical abnormalities. Myxomas typically appear
hyperintense compared with normal myocardium and hypo-
intense compared with the blood pool. Following contrast
agent administration, lesions often show more heterogeneous
enhancements on late gadolinium enhancement.
10,11
In difficult
cases, both TEE and cardiac magnetic resonance imaging may
be helpful for follow up.
Complete surgical removal of the tumour and its cardiac
attachment is usually curative. Excision of the underlying atrial
septum with shaving off of part of the myocardium (at least 5-mm
margin all around) underlying the stalk is necessary during primary
myxoma excision for the prevention of recurrence; closure with
untreated autologous pericardium is dictum in all atrial myxoma
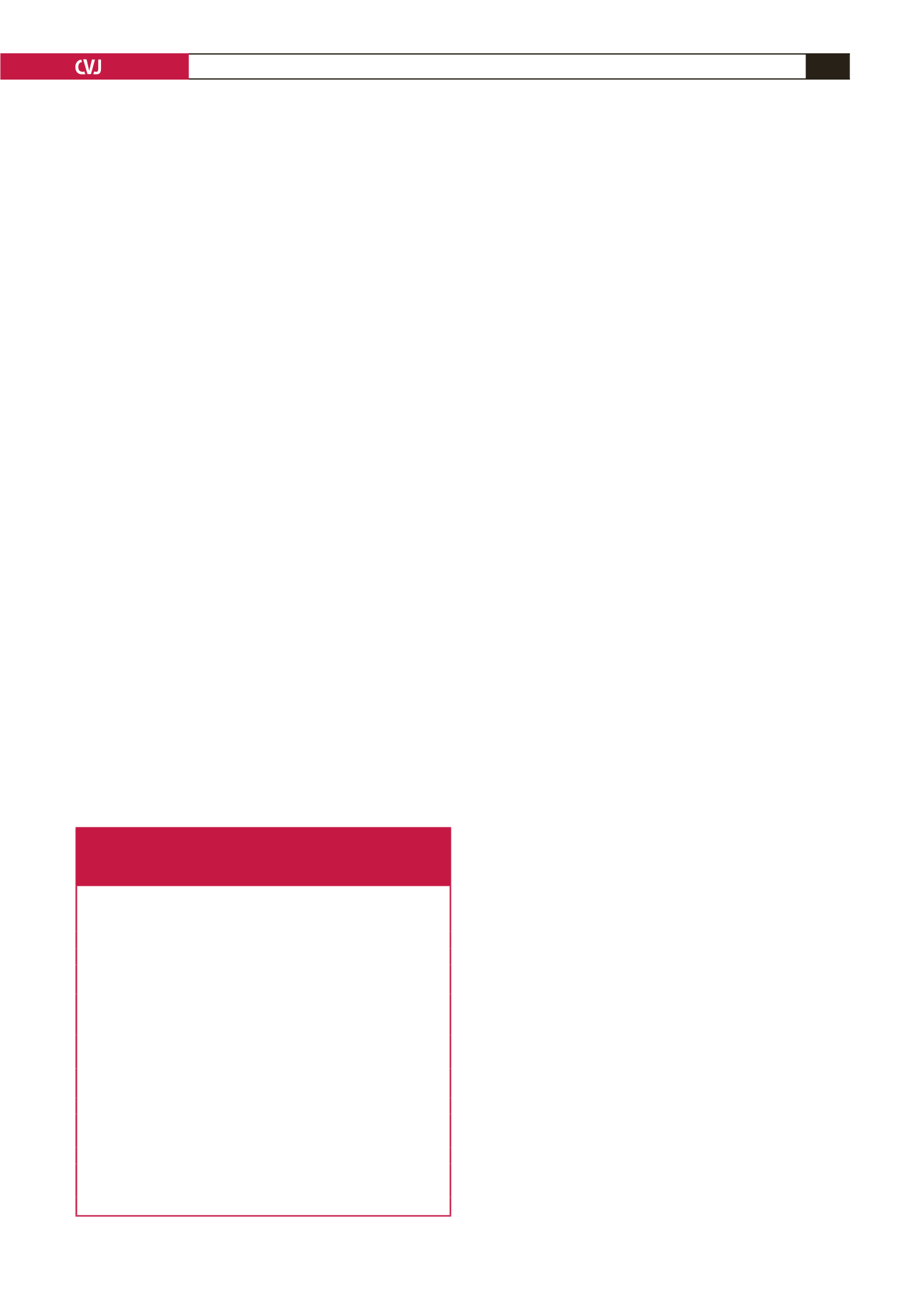
Table 1. Diagnostic criteria for Carney complex.
A patient with Carney complex must either exhibit two of the
manifestations of the diseases listed, or exhibit one of these
manifestations and meet one of the supplemental criteria
Manifestations
1.
Spotty skin pigmentation with typical distribution (lips, conjuntiva and
inner or outer canthi, vaginal and penile mucosa)
2.
Myxoma (cutaneous and mucosal)
3.
Cardiac myxoma
4.
Breast myxomatosis or fat-suppressed magnetic resonance imaging find-
ings suggestive of this diagnosis
5.
Primary pigmented nodular adrenal disease or paradoxical positive
response of urinary glucocorticosteroids to dexamethasone administra-
tion during Liddle test
6.
Acromegaly due to growth hormone-producing adenoma
7.
Large cell-calcifying Sertoli cell tumour
8.
Thyroid carcinoma or multiple, hypo-echoic nodules on thyroid ultraso-
nogaphy in a young patient
9.
Psammomatous melanotic Schwannoma
10. Blue nevus
11. Breast ductal adenoma
12. Osteochondromyxoma
Supplemental criteria
1.
Affected first-degree relative
2.
Inactivating mutation of the PRKAR1A gene

















