CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 4, July/August 2010
AFRICA
193
importance of antithrombotic therapy for their medical condi-
tion, if their managing physician had suggested they start on
anticoagulation therapy, and if this was so, if the patient had
declined anticoagulant treatment.
Echocardiographic studies
Conventional TTE and TEE were carried out in the presence of
two skilled cardiologists using the Philips ie33 system. The TTE
measurements were obtained from the parasternal long-axis view
by two-dimensional targeted M-mode tracing according to the
recommendations of the American Society of Echocardiography.
TEE was performed using a multiplane probe with a 7.0-MHz
transducer.
All patients had fasted on the day of the TEE procedure. They
were put under conscious sedation by intravenous Midazolam
injection, which was given in a range from 1.5–5 mg. Topical
anesthesia of the hypopharynx was achieved by lidocaine spray.
The left atrial appendage (LAA), as the major location of
cardiac thrombi in patients with chronic non-valvular atrial
fibrillation, was visualised from the two-chamber longitudinal
view of the left atrium and left ventricle. Thrombus was defined
as the presence of a distinct, well-contoured echogenic mass,
identified in at least two different views. The presence of spon-
taneous echo contrast (SEC) was described as dynamic ‘smoke-
like’ echoes with swirling motion in the cavity. The impact of the
white-noise artifact was excluded by adjusting the gain setting
as required.
After the procedure, all acquired trans-oesophageal images
were carefully explained to the patient and a companion. After
elaborating on the possible consequences of the pathologies that
were detected, patients were advised to start on anticoagulation
treatment.
Statistical analysis
All values were expressed as means
±
SD or fractions. Statistical
analyses were performed using statistical software (SSP, version
2.80, 2005).
Results
Seventy patients with chronic atrial fibrillation took part in this
study. Mean patient age was 65.85
±
10.02 years, and 68.57%
were women. Other baseline patient characteristics are shown
in Table 1. None of the patients was taking warfarin prior to the
study; 61 (87.14%) patients were on aspirin before entering the
study.
Forty-eight (68.57%) patients were not aware of the impor-
tance of anticoagulation therapy for their condition. Thirty-six
(51.43%) patients admitted that were advised by their physi-
cian to start on anticoagulation therapy. Patient refusal to take
warfarin was mostly because of the fear of haemorrhage or the
inconvenience of INR monitoring, due to frequency of monitor-
ing or distance of the INR monitoring centre from the patient’s
residence.
Mean left atrial diameter of the included patients was 51.74
±
7.46 mm. SEC was present most frequently in the left atrium (in
64.29% of patients). Fifty-two (74.29%) patients had SEC in the
left or right atrium, whereas 33 (47.14%) had SEC in both atria.
Thrombi were found most frequently in the left atrial appendage
(25 cases) (Table 2), whereas 32 (45.71%) patients had thrombi
in either the left or right atrial appendage. Additional trans-
oesophageal data are presented in Table 2. Fifty-four (77.14%)
patients had thrombi or SEC in at least one of their supraven-
tricular cavities.
The mean follow-up period was 23.76
±
2.8 months. During
this period, one patient died as a consequence of ischaemic
stroke. TEE was performed one month prior to the event and the
deceased 66-year-old female was diagnosed with LAA throm-
bus, as well as the presence of SEC in both atria. One patient
suffered an ischaemic stroke and two patients experienced tran-
sient ischaemic attacks over the follow-up period. Two patients
were hospitalised due to signs and symptoms of heart failure.
Following the procedure and after thorough explanation of the
TEE findings to the patients, we managed to start anticoagulation
therapy on 60 (85.71%) patients. Thirty-five (50%), in addition
to warfarin, took low-dose aspirin. The 10 (14.29%) patients who
did not agree to start on anticoagulation with warfarin settled for
thrombo-prophylaxis with aspirin.
At the end of the follow-up period, 53 (75.71%) patients
remained on warfarin therapy. Five had stopped the anticoagula-
tion regimen due to minor bleeding problems, while two patients
had preferred to stop warfarin therapy due to an inability to have
regular INR monitoring. However, these patients agreed to take
low-dose aspirin.
Discussion
Non-valvular atrial fibrillation increases the risk of stroke
four- to fivefold in all age groups,
1,7
with the main source of
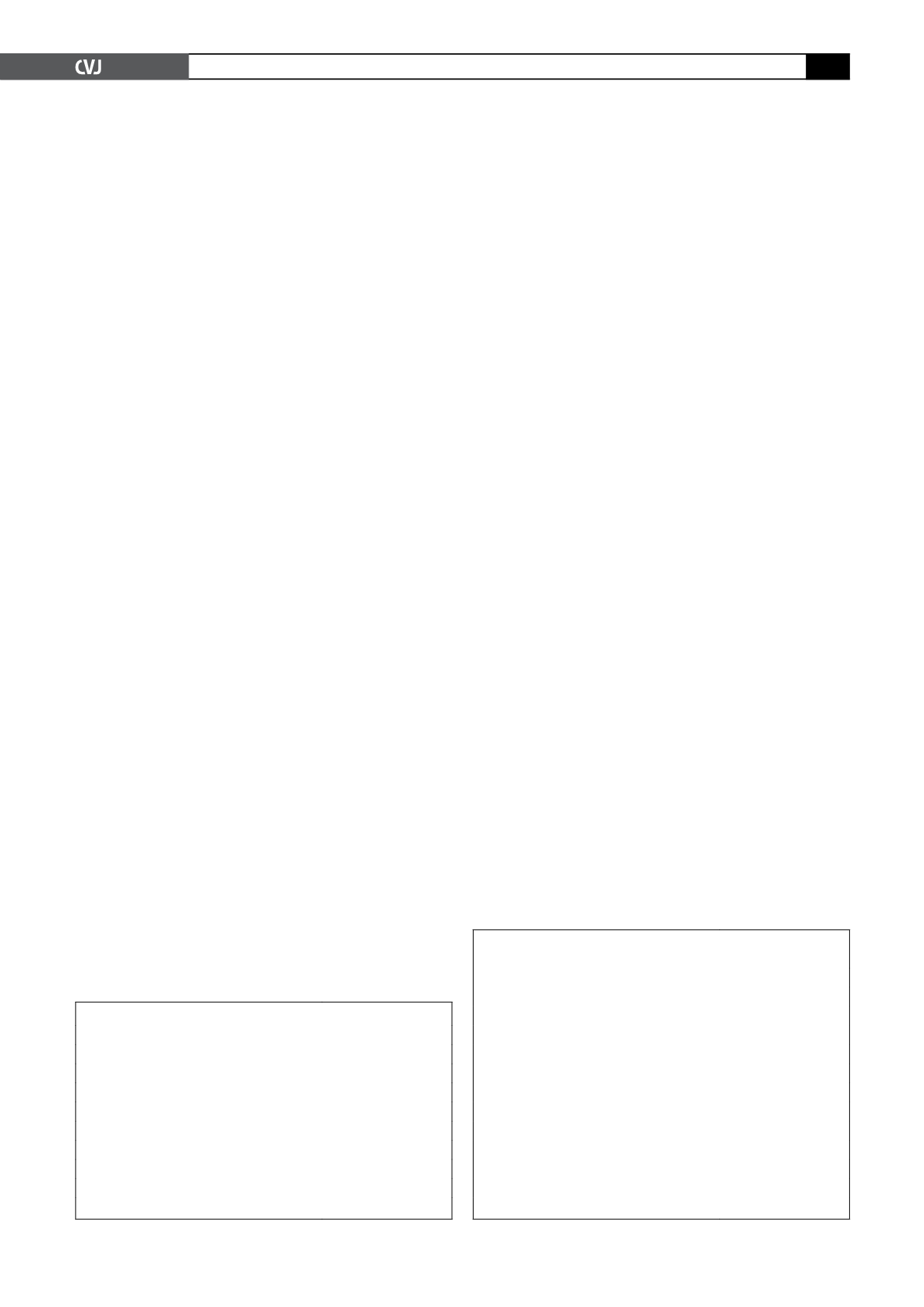
TABLE 1. BASELINE PATIENT CHARACTERISTICS
n
=
70
Age (years)
65.85
±
10.02
Female (%)
48/70 (68.57)
Male (%)
22/70 (31.43)
Hypertension (%)
54/70 (77.14)
Coronary artery disease (%)
29/70 (41.43)
Diabetes mellitus (%)
25/70 (35.71)
Heart failure (%)
20/70 (28.57)
History of stroke (%)
9/70 (12.86)
Data are presented as mean
±
SD or
n
(%).
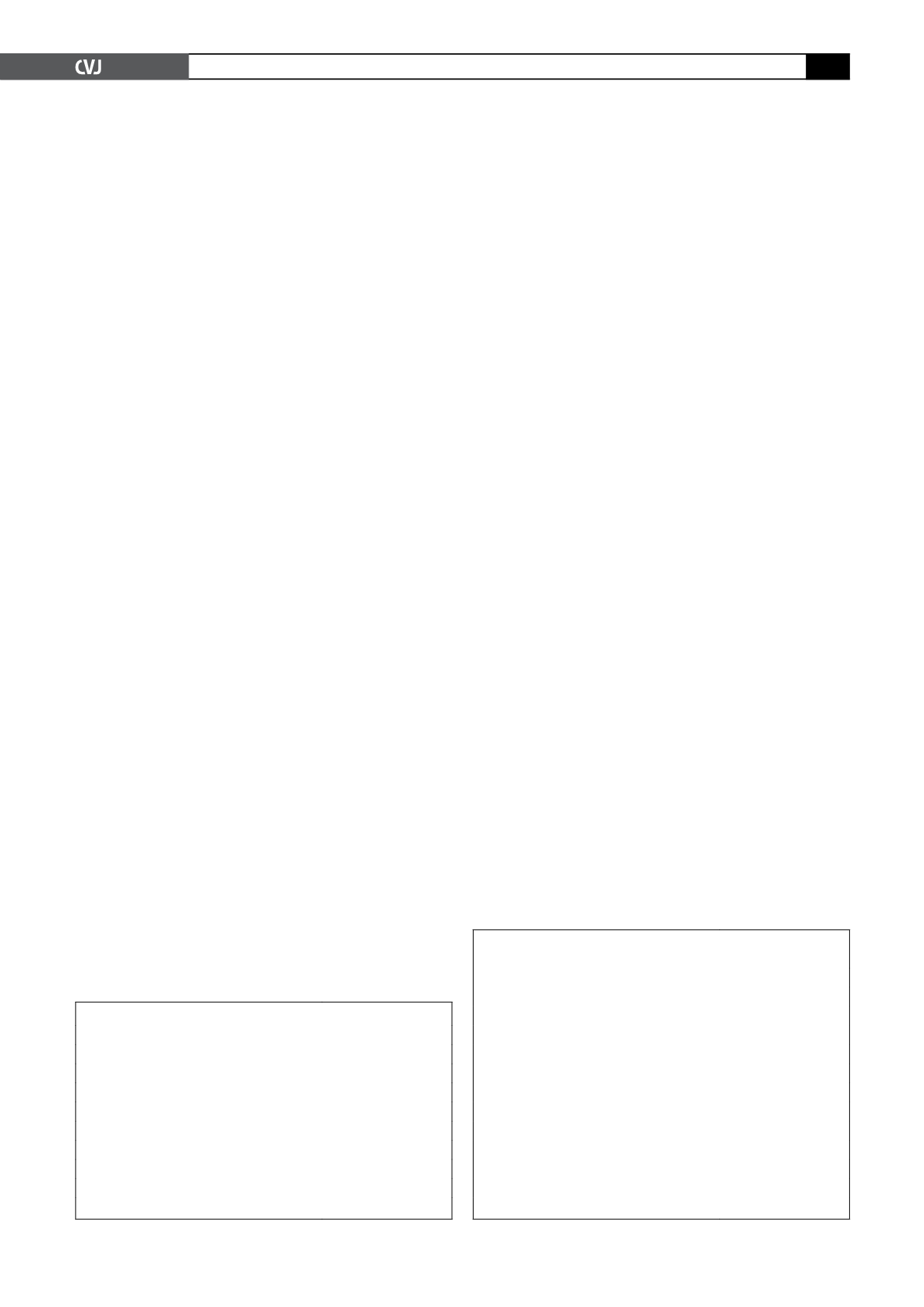
TABLE 2. TRANS-OESOPHAGEAL DATA
OF THE PATIENT POPULATION
n
=
70
LAD, TEE (mm)
51.74
±
7.46
LAA maximal area (cm
2
)
4.3
±
1.93
RAA maximal area (cm
2
)
0.99
±
0.6
LA SEC (%)
45/70 (64.29)
RA SEC (%)
40/70 (57.14)
LA or RA SEC (%)
52/70 (74.29)
LA and RA SEC (%)
33/70 (47.14)
LAA thrombus (%)
25/70 (35.71)
RAA thrombus (%)
15/70 (21.43)
LAA or RAA thrombus (%)
32/70 (45.71)
LAA and RAA thrombus (%)
8/70 (11.43)
Data are presented as mean
±
SD or
n
(%).