CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 6, November/December 2010
336
AFRICA
Apart from measuring pulmonary artery systolic and dias-
tolic pressure from the tricuspid and pulmonary regurgitant
jets, respectively, echocardiography allows exclusion of left
heart pathology and congenital shunts as possible aetiologies.
Additionally, right ventricular size and function, which have
important prognostic value, may be derived using a variety of
indices. The echocardiographic definition of PH is a pulmonary
artery systolic pressure greater than 40 mmHg.
Once suspected, a series of investigations should be under-
taken (Fig. 4) in order to define the cause of PH. The sequence
of testing indicated in the algorithm serves merely as a guideline
– investigations should be guided by the most cost-effective
approach and based on sound clinical judgment.
The classification of PH has undergone a series of modifi-
cations since the original description endorsed by the WHO in
1973, with the latest proposal published from a symposium held
in Dana Point, California.
4
The classification essentially seeks
to create categories of PH that share pathological and clinical
features and have similar therapeutic options and is summarised
in Table 1.
Is cardiac catheterisation indicated in every patient
with suspected PAH?
Despite advances in non-invasive imaging, including echocardi-
ography, CT and MRI, invasive left and right heart catheterisa-
tion is imperative to confirm pulmonary hypertension, rule out
passive (category 2) aetiologies and intra-cardiac shunts, assess
for acute vaso-reactivity and for prognostication purposes.
Pulmonary angiography is not routinely necessary but may
be useful to exclude thrombo-embolic disease, vasculitis and
peripheral pulmonary artery stenosis.
The haemodynamic definition of PAH is a mean pulmonary
artery pressure greater than 25 mmHg at rest or 30 mmHg with
exercise, with a pulmonary capillary wedge pressure or left
ventricular end-diastolic pressure less than 15 mmHg and a
pulmonary vascular resistance greater than 3 ru. When there are
marked respiratory variations in wedge pressure, values should
be measured at end-expiration.
Oxygen and inhaled nitric oxide (10–30 ppm) are the most
useful agents for acute vaso-reactivity testing in the catheterisa-
tion laboratory. Inhaled nitric oxide has the advantage that it
acts selectively on the pulmonary circulation, since it is rapidly
inactivated by haemoglobin on entry into the blood stream and it
does not cause ventilation–perfusion mismatch because it is only
distributed to lung segments that are normally ventilated.
Only 5 to 10% of patients subjected to vaso-reactivity testing
are classified as responders, variously defined as an absolute
reduction in mean pressure greater than 10 mmHg to a mean
value less than 40 mmHg, or a greater-than 20% reduction in
mean pressure and pulmonary vascular resistance.
9
What is optimal medical therapy for PAH?
General measures for patients with PAH include limitation of
physical effort, vaccination against influenza and home oxygen
for hypoxic individuals. Although not supported by rigorous
evidence, prophylactic warfarin anticoagulation, diuretics for
those with systemic venous congestion and digitalis for right
ventricular dysfunction may be appropriate. Women of child-
bearing age should be strongly discouraged from falling preg-
nant since maternal mortality is in excess of 50%, and should
utilise appropriate techniques for contraception.
Patients identified as acute responders on vaso-reactivity
testing benefit from high-dose dihydropyridine calcium antago-
nists but should be monitored closely since about one-half may
relapse in the long term. Empirical use of calcium antagonists
without vaso-reactivity testing, a practice that is not infrequent,
should be strongly discouraged.
Current therapy specifically targeted at PAH comprises the
prostanoids, endothelin antagonists and phosphodiesterase type-
5 inhibitors. The prostanoids may be administered intravenously
(epoprostenol, trepostinil and iloprost), subcutaneously (treposti-
nil), by inhalation (iloprost) or orally (beraprost). Endothelin
antagonists may cause non-specific blockade of both the type
A and B receptor (bosentan) or selective inhibition of the type
A receptor (sitexantan and ambrisentan). The phosphodiester-
ase type-5 inhibitors (sildenafil, revatio and tadalafil) increase
nitric oxide availability by inhibiting the breakdown of the
second messenger, cyclic guanosine monophosphate. For a more
detailed account of these drugs the reader is referred to a recent
review,
10
but unfortunately, apart from the phosphodiesterase
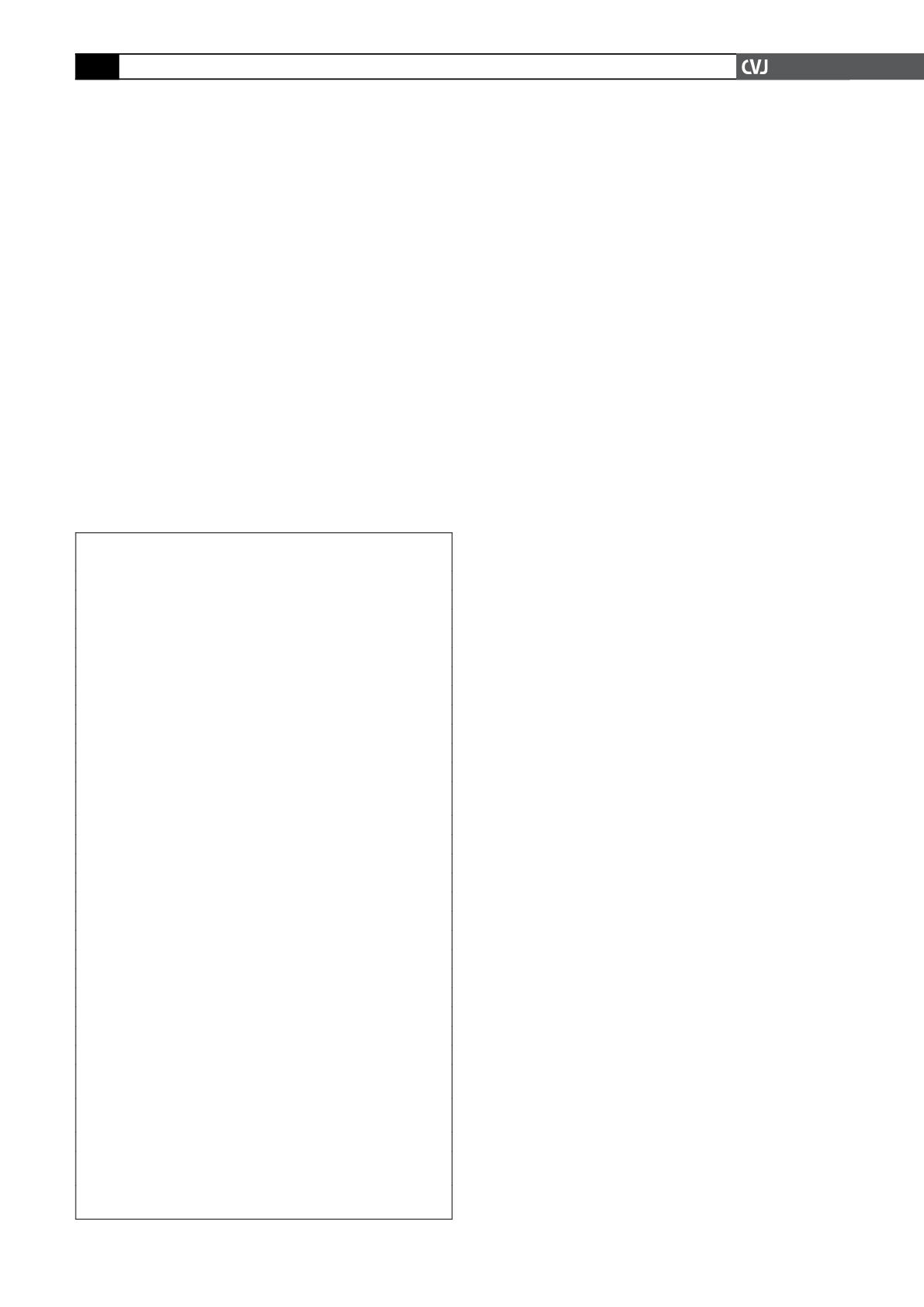
TABLE 1. UPDATED CLINICAL CLASSIFICATION OF
PULMONARY HYPERTENSION (DANA POINT, 2008)
1 Pulmonary arterial hypertension (PAH)
1.1 Idiopathic
1.2 Heritable
1.3 Drugs and toxin induced
1.4 Associated with (APAH)
1.41 Connective tissue disease
1.42 HIV infection
1.43 Portal hypertension
1.44 Congenital heart disease
1.45 Schistosomiasis
1.46 Chronic haemolytic anaemia
1
′
Pulmonary veno-occlusive disease and/or pulmonary capillary
haemagiomatosis
2 Pulmonary hypertension due to left heart disease
2.1 Systolic dysfunction
2.2 Diastolic dysfunction
2.3 Valvular disease
3 Pulmonary hypertension secondary to lung disease and/or hypoxia
3.1 Chronic obstructive pulmonary disease
3.2 Interstitial lung disease
3.3 Lung diseases with mixed restrictive and obstructive patterns
3.4 Sleep-disordered breathing
3.5 Alveolar hypoventilation disorders
3.6 Chronic high-altitude exposure
3.7 Developmental abnormalities
4. Chronic thrombo-embolic pulmonary hypertension
5. Pulmonary hypertension with unclear and/or multifactorial mecha-
nisms
5.1 Haematological disorders: myeloproliferative disorders, sple-
nectomy
5.2 Systemic disorders: sarcoidosis, neurofibromatosis, vasculitis
5.3 Metabolic disorders: glycogen storage disease, Gauchers,
thyroid disorders
5.4 Others: tumour obstruction, fibrosing mediastinitis, chronic
renal failure on dialysis