CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 4, May 2012
AFRICA
195
interviews. The average follow-up period was 35
±
11 (23–56)
months.
In statistical analysis, values were expressed as mean
±
standard deviation for continuous variables, and number and
percentage for dichotomous variables. In comparisons, the
Student’s
t
-test was used for continuous variables and the Mann-
Whitney
U
-test for dichotomous variables. Comparison of
gender was done using the Chi-square test. A
p
-value below 0.05
was set as significant.
Results
There were a total of 15 patients, 11 were male and four female.
Their pre-operative data are summarised in Table 1. Mean age
was 65
±
14 (range 27–76) years. The mean time interval from
the diagnosis of the haematological malignancy to the CABG
surgery was 4.6 years (7 months to 9 years). All were in remission
and under supervision of the Haematology Department.
An average of 2.75
±
1.2 grafts was placed in the 15 patients
undergoing isolated CABG. LIMA grafts were used in 14
patients. All were operated on with an arrested heart under CPB.
Two patients required intra-aortic balloon pump during the peri-
operative period. Haematology reports reflected the expected
ranges in all patients during the postoperative period.
In patients with CLL and NHL, the average length of stay in
ICU was 1.2
±
0.3 and 1.5
±
0.5 days, respectively. The average
of packed red blood cells required was 2.1
±
0.6 and 1.5
±
0.6 units, respectively, and the average of fresh frozen plasma
required was 1.3
±
0.5 and 1.5
±
0.6 units, respectively. There
was no apparent difference in the postoperative course and mean
postoperative stay between the two groups (Table 2).
Four postoperative complications occurred in four patients
(26%). Three of them required early re-operation because of
bleeding. They were respectively, 55-, 63- and 69-year-old male
patients, diagnosed with NHL. More bleeding was seen in the
patients with NHL than in those with CLL, and the difference
was statistically significant (
p
<
0.05). The hospital stay was
uneventful after the second operation.
A 27-year-old male patient diagnosed with CLL was
hospitalised one month after the first operation due to
mediastinitis. This patient was treated with antibiotics according
to bacterial culture and he then underwent sternal dehiscence
revision surgery. The hospital course was uneventful after
the second operation and he soon returned to work. Clinical
and peri-operative variables of patients with CLL and NHL
were similar (Tables 1, 2). No mortality was seen in the early
postoperative period.
The three-year survival rate was 80%. There were five (33%)
late deaths during the follow-up period. All deaths were of a
non-cardiac nature. Three patients were lost due to intracranial
bleeding in the 16th, 23rd and 38th months after surgery. The
other two patients had sudden death in the eighth and 55th
months and the reason for death could not be determined. One
of these patients was brought to the emergency department with
cardiopulmonary arrest. Resuscitation was performed but the
patient died and the family refused an autopsy.
Discussion
Haematological malignancies, particularly the lymphocytic
types, affect mainly elderly patients. Survival of these patients
can range from one year to several decades.
2,5
Over the past few
years, treatment options have continued to improve survival rates.
Cardiac surgical experience in patients with haematological
malignancies is limited and detailed investigation is mandatory
in decision making.
2
It is obvious that CPB affects all systems, including the
haematopoietic system. CPB, which aggravates cell damage,
also has immune-depressant properties, resulting in an
increased incidence of infection.
6,7
Furthermore, haematological
malignancies may lead to antibody deficiency, leucopenia or
impaired T-cell function. Previous reports demonstrate infection
as the primary cause of morbidity.
2,3,8
Some studies show
morbidity rates of between 23 and 57%. Samuels
et al
. reported
the incidence of infectious complications as 42%, underlining the
major role they play in the hospital stay.
2,5
Some investigations
emphasise the use of additional intravenous immunoglobulin,
as broad-spectrum antibiotic prophylaxis was found to be
insufficient to prevent or control infection in these patients.
2
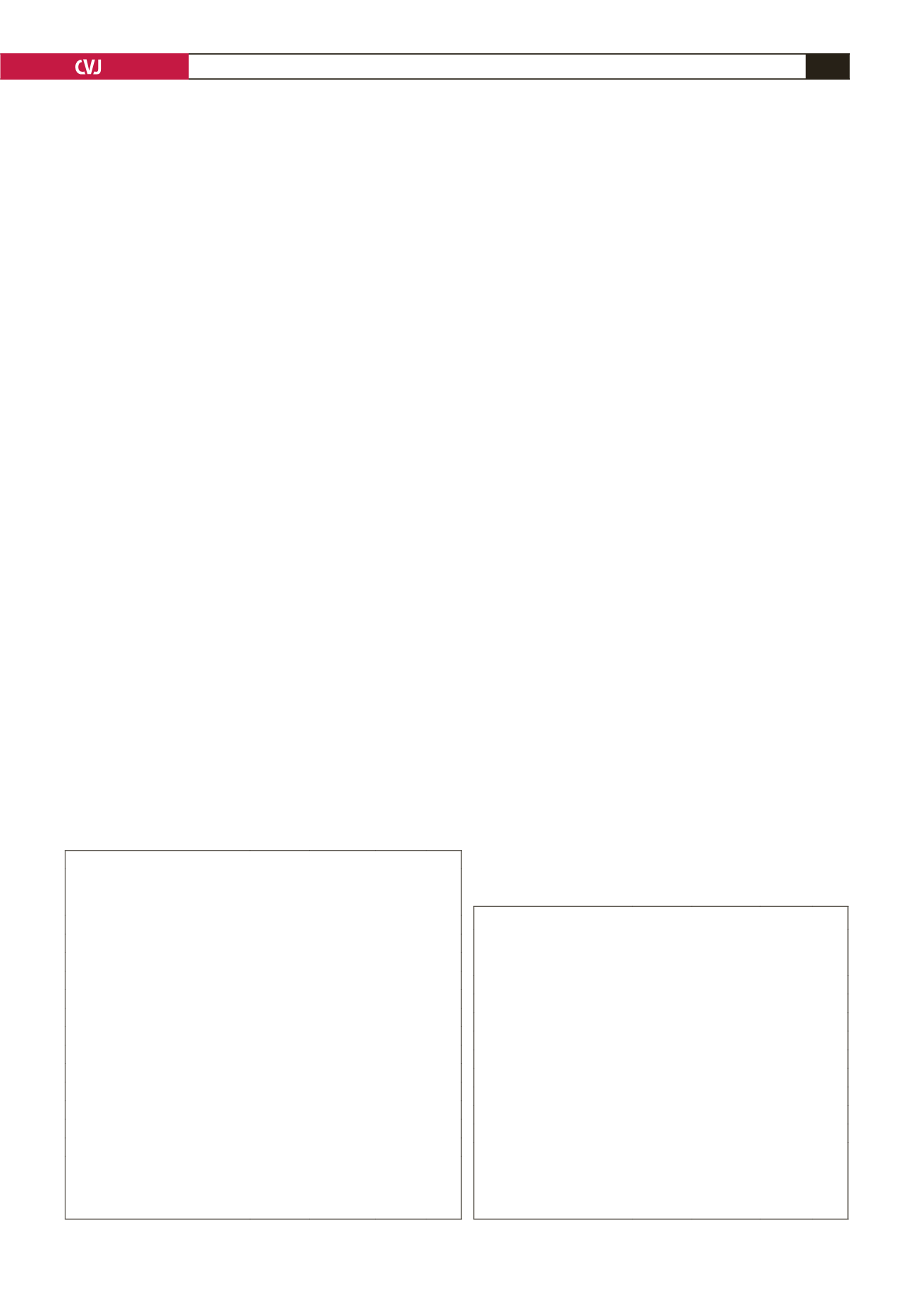
TABLE 2. PERI-OPERATIVE DATA
Diagnosis
CLL
Non-
Hodkgin’s
lymphoma
p
-value CML
CPB time (min)
83
±
21 88
±
16 0.215* 95
Cross-clamp time (min)
64
±
19 69
±
24 0.083* 72
Packed red blood cells (units) 2.1
±
0.6 2.3
±
0.8 0.573** 3
Fresh frozen plasma (units)
1.3
±
0.5 1.5
±
0.6 0.755** 1
Post-operative IABP
1
1
0.950** –
ICU stay (days)
1.2
±
0.3 1.5
±
0.5 0.491* 1
Mortality early/late
–/3
–/2
0.950** –
Bleeding complications
–
3
0.030**
Infection
1
–
0.755**
CLL: chronic lymphocytic leukaemia, CML: chronic myelocytic leukae-
mia, CPB: cardiopulmonary bypass, IABP: intra-aortic balloon pump,
ICU: intensive care unit, *Student’s
t
-test, **Mann-Whitney
U
-test,
p
-value represents the comparison between CLL and non-Hodkgin’s
lymphoma patients.
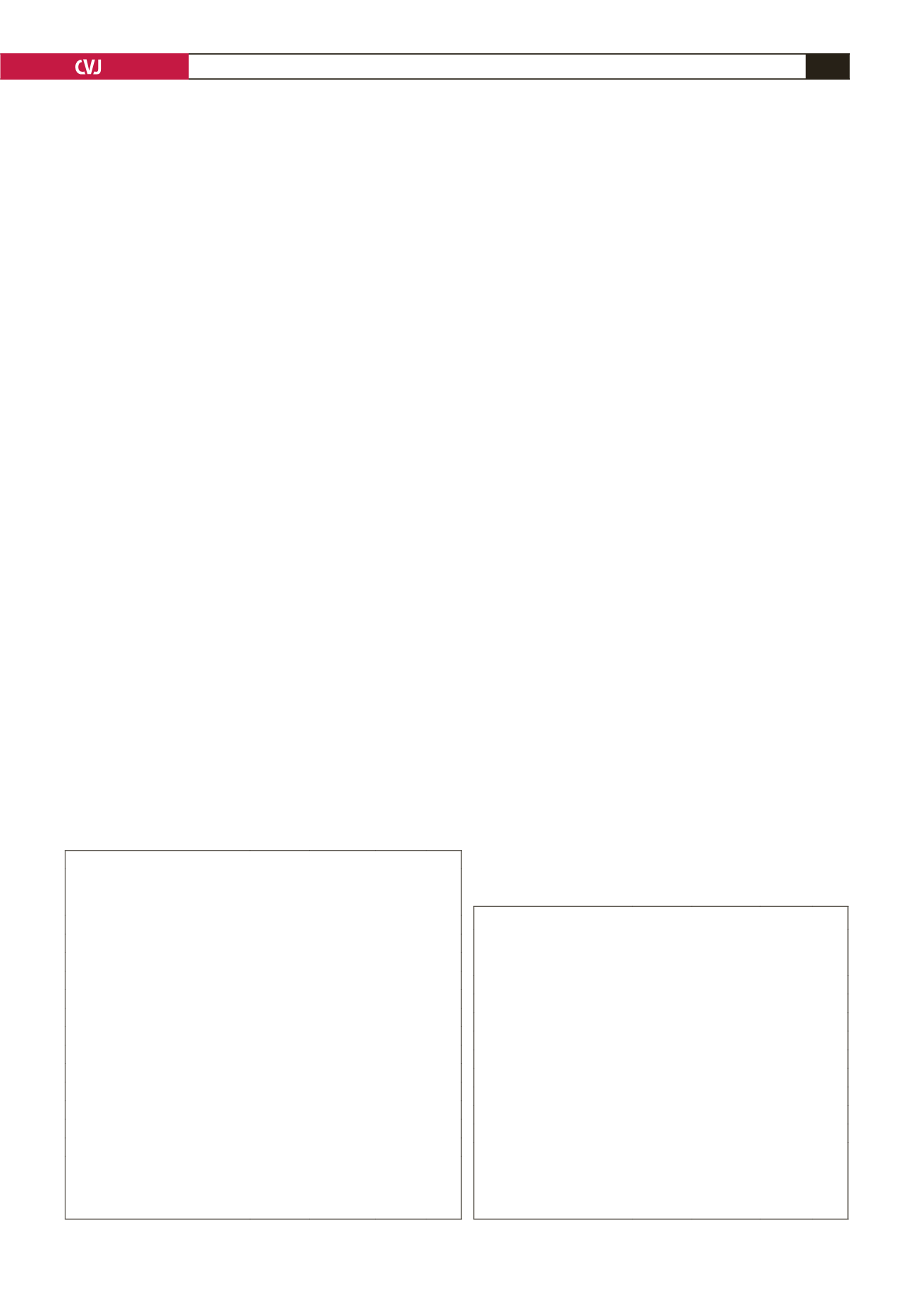
TABLE 1. CLINICAL DATA
Diagnosis
CLL
Non-
Hodkgin’s
lymphoma
p
-value CML
Number
8
6
1
Gender (male/female)
6/2
4/2 0.733 0.733** M
Age (years)
66
±
16 60
±
12 0.128* 78
Body mass index
24
±
4.2 26.5
±
4.9 0.096* 22
Pre-operative EF (%)
49
±
13 52
±
18 0.226* 44
Pre-operative haemoglobin (g/dl)
13.3
±
3.6 12.8
±
2.9 0.258* 15.4
Post-operative haemoglobin (g/dl) 11.9
±
7.2 10.8
±
8.6 0.086* 12.3
Pre-operative platelets (
×
109 /dl)
206
±
74 254
±
89 0.068* 139
Post-operative platelets (
×
109 /dl) 174
±
51 152
±
73 0.070* 128
Pre-operative prothrombin time (s) 12.8
±
4.1 12.5
±
2.8 0.825* 13.3
Post-operative prothrombin time (s) 13.2
±
7.2 12.9
±
9.4 0.652* 13.1
Pre-operative WBC (
×
109 /dl)
33.2
±
9.1 38.5
±
10.8 0.075* 20.0
Post-operative WBC (
×
109 /dl)
36.1
±
1.4 34.8
±
5.3 0.348* 17
CLL: chronic lymphocytic leukemia, CML: chronic myelocytic leukemia, EF:
ejection fraction, WBC: white blood cells, Postoperative: 14th day. *Student’s
t
-test, **Chi-square test;
p
-value represents the comparison between CLL and
non-Hodkgin’s lymphoma patients.