CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 4, May 2012
202
AFRICA
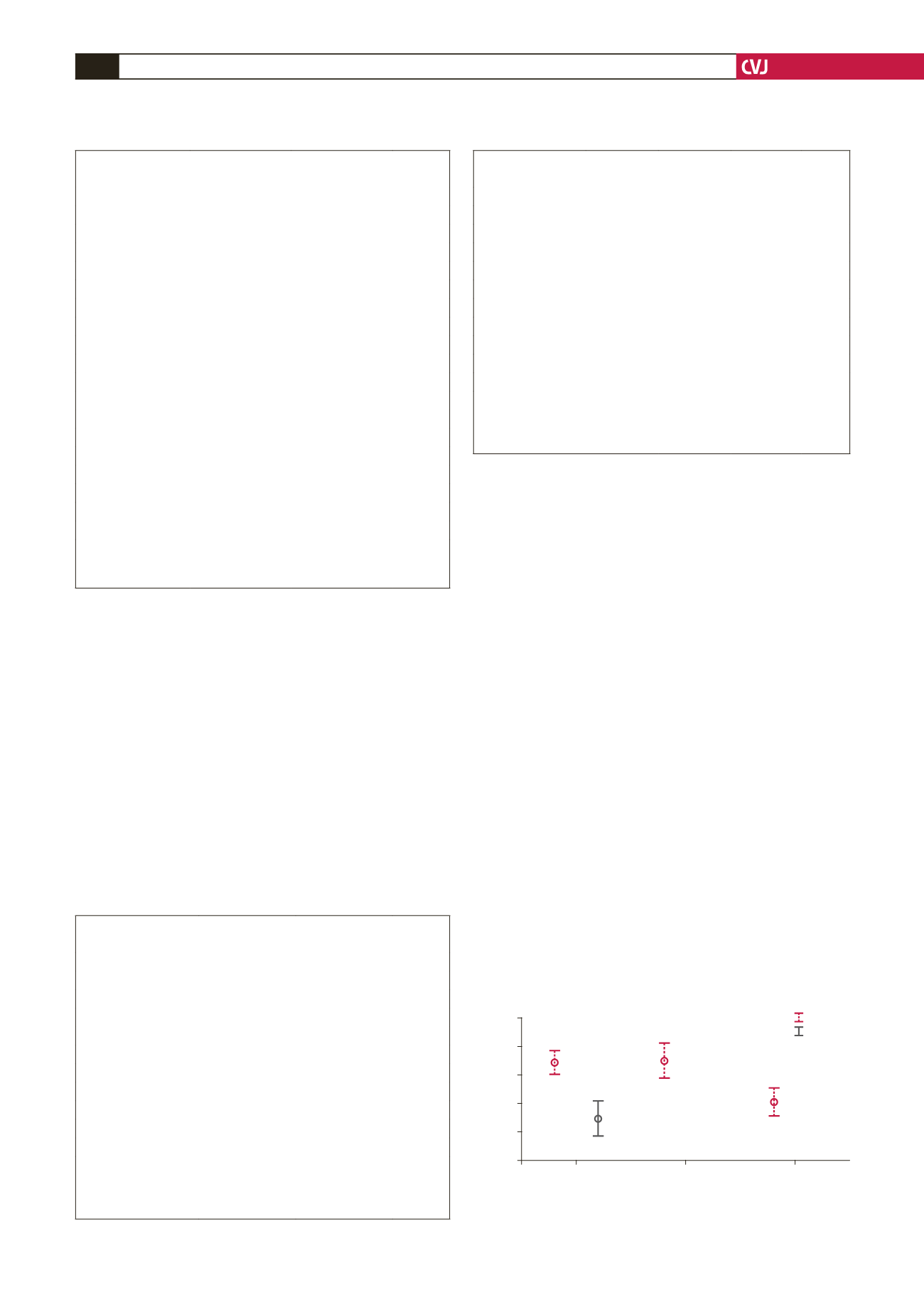
There was an increase in the diastolic filling ratios (Em/Ea) and a
decrease in the TDI systolic wave. The fourth patient had a large
drop in the NT-proBNP level, as well as an increase in the TDI
systolic wave, in keeping with the preserved LV contractility.
There was a small decrease in the ESD post-operatively (Fig.
1). These four were identified by NT-proBNP cut-off levels
set by Januzzi’s rule-in criteria (450 pg/ml, ~53 pmol/l) for the
diagnosis of heart failure in the PRIDE study
6
at six weeks.
A ROC curve was constructed for each variable to assess
its discriminating capacity to distinguish between surgical
cases and controls. The area under the curve was highest for
NT-proBNP; this was the only parameter that approached 90%
(Fig. 2). However, at established cut-off levels for normality,
NT-proBNP (12 pmol/l
=
125 pg/ml) yielded the highest
sensitivity of 96% but had a low specificity of 45%. Using
cut-off criteria established by Januzzi
6
for the detection of
heart failure (NT-proBNP
>
53 pmol/l), the specificity for
NT-proBNP improved to 74%, and the positive predictive value
to 84%. Of interest, eight patients in the control group had BNP
levels
>
53 pmol/l, and of these, six underwent surgery within
the ensuing six months.
A second ROC curve (Fig. 3) was constructed using all the
variables to separate NYHA classes I–II from III–IV. Once
again, NT-proBNP emerged with the highest area under the
curve, followed closely by the ESD. Bivariate analysis was
performed to assess the ability of the different parameters to
predict a favourable outcome, defined arbitrarily as NT-pro BNP
level
<
50 pmol/l. These were an effective orifice area (EOA) (
p
=
0.014), tissue Doppler S wave (
p
=
0.049) and left atrium (LA)
size (
p
=
0.027), all pointing to the interrelationship between
severe regurgitation, systolic function and NT-proBNP levels.
Discussion
This is one of the first studies to use new modalities of
measuring left ventricular function with TDI and NT-proBNP
assays. NT-proBNP level has been shown to be a marker of left
ventricular dysfunction and has been used to predict diastolic
abnormalities in patients with normal systolic function,
7
limiting
the need for expensive cardiac imaging modalities.
8,9
In this
study, NT-proBNP level yielded the highest predictive value for
discriminating between cases selected for surgery and controls
followed up at the cardiology outpatients’ clinic (sensitivity of
96%). The ESD at the established cut-off point of 45 mm that
defines the need for surgery had a higher specificity of 81%.
TABLE 2. BASELINE QUANTIFICATION
OF THE SEVERITY OF MR
Variables
Controls (
n
=
27)
Study (
n
=
27)
p
-value
RF
<
70%
6
2
0.192
70–80%
6
3
>
80%
15
19
RV
>
60 ml
27
27
1.000
EOA
<
0.35
3
1
0.058
0.36–0.40
2
4
0.41–0.90
17
10
>
0.90
5
12
PAS
<
30 mmHg
0
0
0.192
30–39
10
6
40
–
59
16
18
>
60 mmHg
1
4
LA size
<
40 mm
4
0
0.074
40–49 mm
5
2
>
49 mm
20
25
EF
<
50%
0
1
0.123
51–60%
1
5
>
60%
26
21
RF
=
regurgitant fraction; RV
=
regurgitant volume; LA
=
left atrium; RV
=
right ventricle; PAS
=
pulmonary artery systolic pressure; EOA
=
effec-
tive orifice area; EF
=
ejection fraction.
TABLE 3. PRE-OPERATIVE QUANTIFICATION
OF LV FUNCTION
Controls
Study
p
-value
LA size (mm)
59.6
±
13
76
±
16
<
0.001
LA volume (ml)
177
±
119
309
±
183
0.003
EDV (ml)
177
±
69
165
±
48
0.472
ESV (ml)
58
±
25
57
±
25
0.898
EDD (mm)
67
±
6
67
±
9
0.06
ESD (mm)
38
±
9
43
±
8
0.043
EF
65
±
10
67
±
7
1.000
TDI (m/s)
0.09
±
0.02
0.1
±
0.07
0.377
TDI Em/Ea
14
±
8
20
±
8
0.004
NT-proBNP (pmol/l)
57
±
88
262
±
224
<
0.001
LA
=
left atrium; EDV
=
end-diastolic volume; ESV
=
end-systolic
volume; EDD
=
end-diastolic dimension; ESD
=
end-systolic dimen-
sion; EF
=
ejection fraction, TDI
=
tissue Doppler imaging; TDI Em/Ea
=
diastolic filling ratio.
TABLE 4. POST-OPERATIVE EVALUATIONAT
ONEAND SIXWEEKS’ FOLLOW UP
1 week
6 weeks
CI
p
-value
LA size (mm)
64
±
16
58
±
16
2.0; 11.2 0.009
LA volume (ml)
234
±
152 182
±
140 21.2; 82.9 0.003
EDV (ml)
139
±
52 125
±
55
–
15.7; 43.8 0.326
ESV (ml)
86
±
47
73
±
47
–
10.7; 37.5 0.250
EDD (mm)
59
±
9
54
±
8
2.5; 10.2 0.004
ESD (mm)
45.5
±
13 38.7
±
9
12.7; 1.0 0.03
EF
42
±
13
51
±
13
–
17.9;
–
1.0 0.0032
TDI syst (m/s)
0.07
±
0.016 0.07
±
0.015
–
0.01; -0.2 0.821
TDI Em/Ea
12
±
4
15
±
3
–
6.7;
–
0.2 0.418
NT-proBNP (pmol/l) 395
±
460 94
±
161 87.5; 514.1 0.009
LA
=
left atrium; EDV
=
end-diastolic volume; ESV
=
end-systolic
volume; EDD
=
end-diastolic dimension; ESD
=
end-systolic dimen-
sion; EF
=
ejection fraction, TDI
=
tissue Doppler imaging; TDI Em/Ea
=
diastolic filling ratio.
Fig. 1. NT-pro BNP time-course changes.
3.00
2.50
2.00
1.50
1.00
0.50
95% CI log BNP (pmol/l)
Baseline
1st week post op 6 weeks post op
Time points
case
control