
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 1, January/February 2015
14
AFRICA
Dash
et al
., 1977,
17
and validated by Califf
et al
.,1985,
18
detects
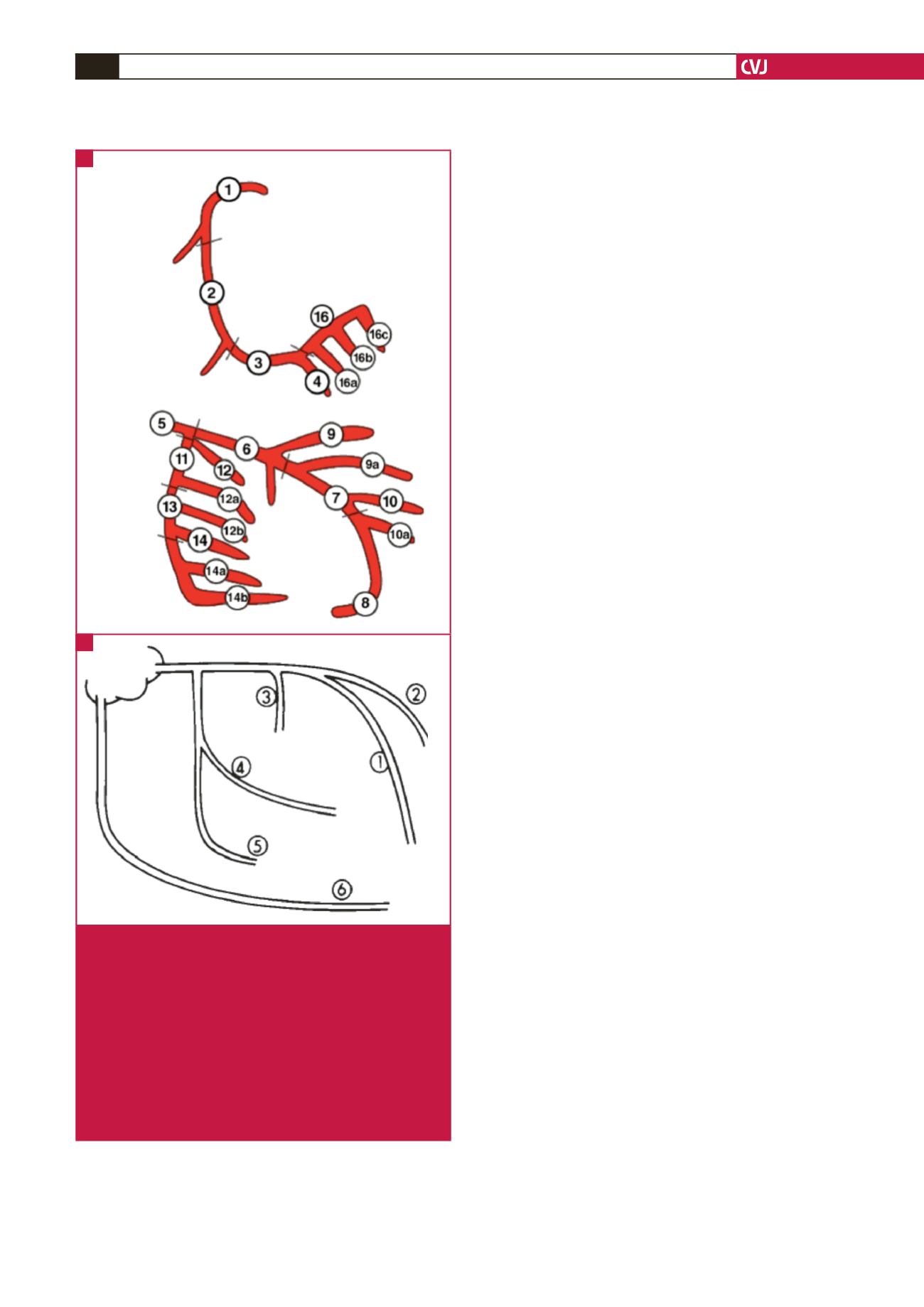
the main vessels affected in their large branches, Fig. 1B).
Coronary angiographies of patients were reviewed by two
experts who were blinded to the patients’ BMI and WHR.
Patients were divided into five groups according to their BMI;
normal BMI (21–24 kg/m
2
), overweight (25–29 kg/m
2
), class I
obesity (30–34 kg/m
2
), class II obesity (35–39 kg/m
2
) and class III
obesity (
>
40 kg/m
2
). Also patients were divided into four groups
according to their age; 20–39, 40–59, 60–79 and
>
80 years old.
Inclusion criteria were patients over 20 years old who
had definite indications for coronary angiography, based on
their clinical background. The exclusion criteria were patients
unwilling to participate in the study.
For the purpose of multivariate analysis, we included in the
study evaluations of conventional cardiovascular risk factors,
such as HTN (systolic blood pressure
≥
140 mmHg and/
diastolic blood pressure
≥
90 mmHg), DM [fasting blood sugar
>
126 mg/dl (6.99 mmol/l) and/glycosylated haemoglobin (HbA
1c
)
>
6%], hyperlipidaemia [low-density lipoprotein (LDL) cholesterol
>
120 mg/dl (3.11 mmol/l) and triglycerides
>
150 mg/dl (1.7
mmol/l)], family history of CAD and cigarette smoking (current
smoker: at least five cigarettes/day for
≥
one year).
Statistical analysis
For analysing data, SPSS version 15 (USA, Illinois, Chicago) was
used. The Student’s
t
-test was used for comparing quantitative
variables between two groups and the one-way ANOVA test was
used for comparing means of quantitative variables between
groups. Logistic regression was used for multivariate analysis of
compounding factors. Chi-square and Fisher’s exact tests were
used for analysis of qualitative variables and a
p
-value
≥
0.05 was
considered significant.
Results
Of 414 (100%) patients, 250 (60.4%) were male and their ages
ranged from 25 to 84 years. The prevalences of DM, HTN,
hyperlipidaemia, family history of CAD and cigarette smoking
were 27.3, 29.5, 39.1, 5.8 and 26.3%, respectively. Basic clinical
and demographic characteristics of the patients are presented in
Table 1.
The severity of CAD was measured by the SYNTAX and
Duke jeopardy scores. For the SYNTAX score, the mean
±
SD of the patients’ scores was 17.7
±
9.6 (range 0–64) and
for the Duke score, it was 3.2
±
1.7 (range 0–12). There was a
negative correlation between the SYNTAX and Duke scores
(severity of CAD) and the patients’ BMI (
p
=
0.01 and
p
=
0.001,
respectively).The correlation between the patients’ BMI and the
severity of CAD (SYNTAX and Duke scores) is presented in
Table 2.
There was an inverse relationship between obesity and the
severity of CAD, according to the SYNTAX and Duke criteria,
which has been defined as the ‘obesity paradox’. In order to rule
out the impact of other cardiovascular risk factors, multivariate
regression analysis was performed. Regression analysis revealed
a
β
-coefficient of –0.14 for the Duke score and –0.17 for the
SYNTAX score. This means that for every unit increase in BMI
there would be a 0.14 and 0.17 decrease in the severity of CAD
according to the Duke and SYNTAX scores, respectively. After
adjusting for confounding factors, there was still a significantly
negative correlation between BMI and severity of CAD (
p
=
0.028 and 0.01, respectively). Meanwhile multivariate analysis
Coronary artery segment
RCA
LCA
LCA
LAD
PDA
RCA
SEPT
CFX
CFX-MARG
LAD DIAG
Fig. 1.
Diagrams of coronary artery tree demonstrating the
16 segments counted in the SYNTAX score (A), and
six segments counted in the Duke jeopardy score (B).
CFX = left circumflex coronary artery; CFX-MARG =
major marginal branch of the left circumflex coronary
artery; LAD = left anterior descending artery; LAD
DIAG = major diagonal branch of the left anterior
descending artery; LCA = left main coronary artery;
PDA = posterior descending coronary artery; RCA =
right coronary artery; SEPT = major septal perforat-
ing artery.
(Adapted from Sianos,
et al
.
Euro Intervent
2005;
1
: 219–227, and Callif,
et al
.
J Am Coll Cardiol
1985;
5
: 1055.)
A
B



















