
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 3, May/June 2015
128
AFRICA
CKD (OR: 1.77 95% CI: 1.18–2.46) in patients with the MetS
in comparison with those without this risk factor. A similar
increased risk of CKD (OR: 1.55 95% CI: 1.34–1.80) was
reported by Thomas
et al.
28
and Tanner
et al
.,
29
respectively.
Thomas
et al
.
28
indicated that the risk of CKD increased with
the number of individual MetS components. A higher increased
risk of CKD (OR: 2.60 95% CI: 1.68–4.08) in the presence of
the MetS was reported by Chen
et al
.
30
This increased risk of
CKD is thought to rely on MetS-associated insulin resistance
and subsequent oxidative stress and endothelial dysfunction.
27,31,32
SCT was not associated with CKD in the present study.
Conflicting reports exist as to whether SCT is a risk factor for the
development and progression of CKD.
3,5,6-8
Earlier small-scale
reports suggested SCT to be an independent risk factor for CKD
and ESRD.
7,8
Derebail
et al
.
8
observed among 188 ESRD African
Americans on dialysis a greater prevalence of SCT (15 vs 7%,
p
=
0.001) in comparison with that inferred from the newborn
haemoglobinopathy screening programme; they suggested SCT
to be an independent risk factor for CKD.
5
Ajayi
et al
.
10
found in black Africans a greater prevalence of
microalbuminuria and proteinuria in type 2 diabetes patients
with SCT in comparison with those with normal haemoglobin
levels. All these authors speculated that the increased prevalence
of SCT could be due to accelerated progression of kidney disease
either as a direct consequence of SCT or by HbAS enhancing
the deleterious effects of another co-morbid condition, such as
diabetes, hypertension or autosomal polycystic kidney disease
(APKD).
3,5,7,8
With reference to methodological issues inherent in these
cross-sectional studies and the geographical variations in the
prevalence of HbAS, additional examination of SCT has
been suggested in well-characterised, geographically diverse
populations with advanced kidney disease.
5
It may also be
interesting to examine the interaction of SCT with other recently
identified genetic risks for ESRD in black individuals, such as
apolipoprotein 1 (APOL1) and non-muscle myosin heavy-chain
9 (MYH9).
5
In line with the above suggestions, recent studies such as the
present study reported no association between SCT and CKD.
7
Bleyer
et al
.
26
found in 376 African American diabetics that
those with and without SCT had similar eGFR and prevalence
of microalbuminuria. Using multivariate analysis, they noted
no difference in the combined outcomes of peripheral vascular
resistance, retinopathy and renal failure.
In order to determine whether the HbAS genotype is
associated with commonly reported aetiologies of ESRD, Hicks
et al
.
6
evaluated cases (
n
=
3.258) with ESRD attributed to type
2 diabetes and non-diabetes causes, predominantly hypertension
attributed and glomerular disease associated. In addition,
relationships between APOL1 G1/G2 nephropathy risk variants
and non-muscle MYH9 risk variants (E1 risk haplotype) and
SCT were assessed to determine whether interactions between
these genes were present. The SCT genotype frequencies were
similar in the cases (8.7% in non-diabetic and 7.1% in type
2 diabetes ESRD) and the controls (7.2%). No evidence of
association between HbAS and either diabetic or non-diabetic
aetiologies of ESRD was detected in this large sample of African
Americans. In addition, no evidence of APOL1 or MYH9
interaction with SCT was observed.
The authors suggested both APOL1 and HbS to be
associated with susceptibility to nephropathy in autosomal,
recessive patterns, with no evidence of risk for nephropathy in
individuals heterozygous for risk variants (e.g. those with SCT).
6
They concluded that African Americans who have a single
copy of the HbS gene are not at increased risk for developing
non-diabetic or diabetic ESRD or subclinical nephropathy,
relative to unaffected individuals.
6
In addition, nephropathy
risk variants in APOL1 function independently from HbS when
contributing to non-diabetic ESRD.
6
In contrast to earlier, small-
scale reports using high-performance liquid chromatography
(HPLC) to determine HbS, the strengths of this study include
the large sample size and direct genotyping for HbS.
6
The interpretation of the results of our study is confounded
by some limitations. The cross-sectional design of the
study precludes any causal relationship between CKD and
associated risk factors. Moreover, the small sample size did not
allow sufficient power to detect any additional associations.
Definition of reduced kidney function and CKD was based
on a unique determination of serum creatinine. As in earlier
smaller studies, HbS determination was based on HPLC
instead of direct genotyping of HbS. One wonders to what
extent the conclusions of this clinic-based study could be
extrapolated to the general population, given the bias in the
referral of patients. The findings of our study, however, give
some indications about the relationship between SCT and
CKD, highlighting the need for a well-characterised study with
a large sample of CKD patients.
Conclusion
In the present case series of black Africans, SCT did not emerge
as an independent determinant of CKD. Classic CKD risk
factors in isolation or combined as the MetS emerged as the
main determinants of CKD.
The authors gratefully thank Dr Jeremie Muwonga for the use of the facili-
ties at the National Laboratory of the National AIDS Control Program for
the analysis of biological samples. We thank Prof Dr Léon Tshilolo for his
outstanding help in the determination of haemoglobin genotypes at the
Laboratory of Monkole Hospital. We are indebted to the staff of the BDOM
network for their commitment during the study. We thank Dr Kensese of
the General Hospital of Kinshasa for his help during the study, and all the
participants who by their consent made the study possible. We acknowledge
the staff of the University of Kinshasa Hospital, Saint Joseph Hospital, espe-
cially Dr Josée Nkoyi, and the General Hospital of Kinshasa.
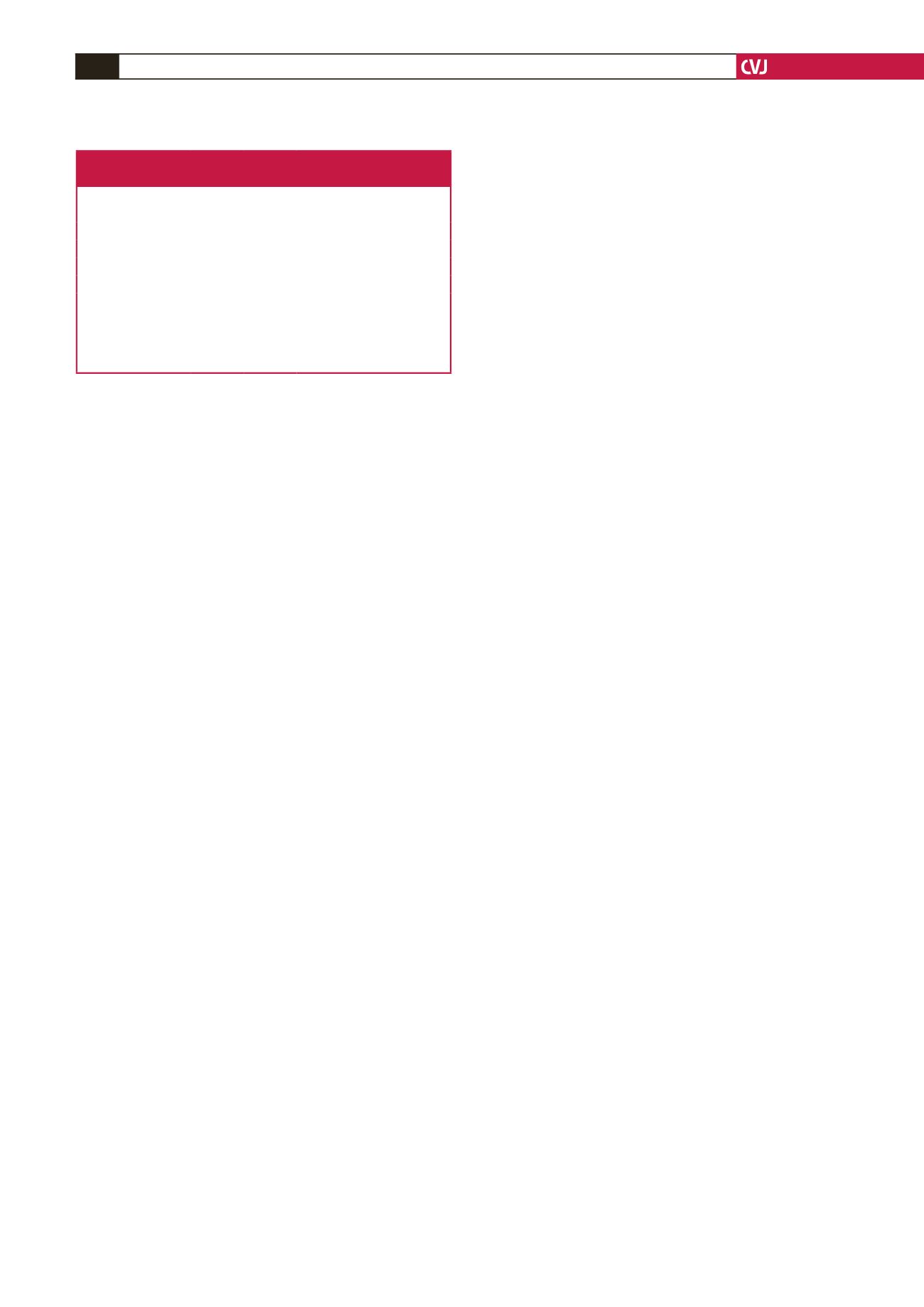
Table 5. Multivariate independent determinants
of chronic kidney disease
Variable
B SE OR (95% CI)
p
-value
Constant
0.227 0.397
–
–
HbAS vs HbAA 0.953 0.810 0.38 (0.559–1.839) 0.235
DM+ vs DM–
1.343 0.282 2.36 (1.150–4.454) 0.001
HT vs NT
0.771 0.300 2.16 (1.202–3.892) 0.001
MetS+ vs MetS–
0.559 0.269 1.69 (1.033–2.965) 0.04
Hb
≥
12 vs 12 g/dl
–1.015 0.278 0.36 (0.220–0.625) 0.001
B, regression coefficient; SE, standard error; OR, odds ratio; Hb,
haemoglobin; HbAS, haemoglobin with sickle cell trait; HbAA,
normal haemoglobin; DM, diabetes mellitus; HT, hypertension; NT,
normotension; MetS, the metabolic syndrome.

















