
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 6, November/December 2015
e6
AFRICA
On the ECG, signs of anterolateral myocardial ischaemia
were observed, and the patient became severely symptomatic.
The dissection, leading to total occlusion of the coronary lumen
without distal antegrade flow, was classified as class F according
to the National Heart, Lung, Blood Institute classification
(NHLBI). A continuous infusion of nitroglycerin and heparin,
as well as a lignocaine infusion, were administered. Within
a few minutes, the patient’s condition stabilised and she was
transferred to the cardiac surgery department.
On admission there, her systolic blood pressure was 110
mmHg and the heart rate was 80 beats/min. The patient
complained of chest pains. Her cardiac necrosis markers were
elevated: creatine kinase-MB (CK-MB) 99 U/l and troponin
T (T
hs
) 449.4 ng/l. The continuous nitroglycerin and heparin
infusion was maintained.
Transthoracic echocardiography (TTE) revealed hypokinesis
of the apex and para-apical segments of the anterior, lateral and
postero-inferior cardiac walls. The ascending aorta was 3.1 cm,
the aortic bulb was 3.2 cm, and signs of dissection on the mitral
side were observed. The ejection fraction was 52%.
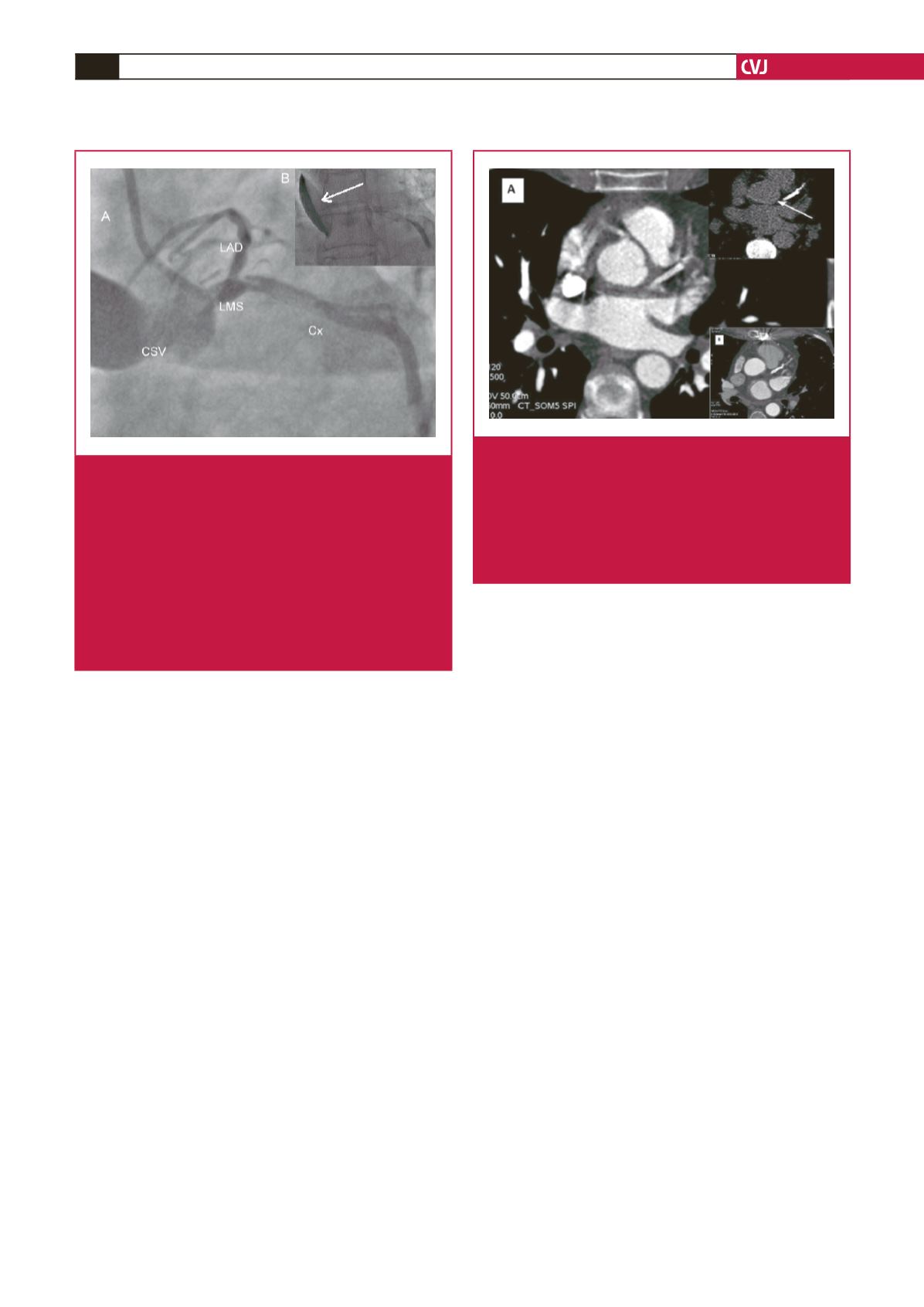
Multi-slice CT (MSCT) angiography showed significant
ostial LMS stenosis (intraluminal diameter 2 mm, area 5 mm
2
) without signs of atherosclerosis. Persistent staining of the
left sinus of Valsalva, extending to the aortic annulus and
non-coronary sinus of Valsalva, was found. The scan indicated
limited aortic dissection (Fig. 2A).
The 12-lead ECG indicated anterolateral STEMI. Laboratory
tests showed significant increase in levels of cardiac markers:
CK-MB 538 U/l and T
hs
7 034 ng/l. A decision was made to
intervene surgically. The time period between the iatrogenic
dissection and surgical intervention was approximately six hours.
An intra-operative view confirmed the presence of a dissection
of the left and non-coronary sinuses of Valsalva. There was
also a haematoma along the proximal portion of the LAD,
which extended to the surrounding epicardium. On a beating
heart, without extracorporeal circulatory assist, total arterial
myocardial revascularisation with double skeletonised internal
thoracic arteries was performed. The right internal thoracic
artery (RITA) was anastomosed to the LAD. The left internal
thoracic artery (LITA) was anastomosed to the Cx. Further
hospitalisation was uneventful.
At the one-year follow up, the patient was feeling well and
remained asymptomatic. Control MSCT angiography (Fig.
2B) revealed complete healing of the limited aortic and LMS
dissection. Competitive native blood flow, the LITA graft
occlusion and the patent RITA graft were also seen on MSCT
angiography.
Discussion
Iatrogenic dissection of a coronary artery during a percutaneous
procedure can be triggered by many factors, including unusual
anatomy of the LMS, atherosclerosis of the LMS, difficulty when
introducing a catheter, vigorous contrast infusion, inexperience
of the operator, catheter type, inappropriate catheter position or
sub-intimal passage of the guidewire.
5
The choice of treatment strategy in the case of an iatrogenic
coronary artery dissection depends on many factors, including
haemodynamic stability, the patient’s clinical state, extension
of the dissection, the number of dissected vessels, and SV
involvement.
5
When dealing with an LMS dissection, urgent
surgical myocardial revascularisation is preferred. Many authors
emphasise the unpredictable nature of a dissected flap.
6
Fig. 2.
A. Multi-slice CT angiography performed during
acute aortic root dissection. Non-enhanced computed
tomography (calcium score sequence) presents a
hyperdense and thickened aortic root wall, which
corresponds to the intramural haematoma (white
arrow). B. At the one-year follow up, control MSCT
angiography showed self-healing of the dissected
aorta. Note the reduced wall thickness.
Fig. 1.
A. Coronary angiogram showing LMS dissection
extending antegradely to the Cx with its distal total
occlusion, and retrogradely to the left and non-coro-
nary SV. A bare-metal stent implanted in the LAD
provided contrast flow. Persistent staining after the
contrast cleared shows the vessel lumen present.
B. Progression of the dissection to almost total contrast
flow occlusion in the left coronary artery branches.
Persistent staining is seen in the false lumen. The
dissection was classified as F according to the NHLBI.
LMS: left main stem, Cx: circumflex artery, SV: sinus of
Valsalva, LAD: lateral anterior descending artery.

















