CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 1, January/February 2016
AFRICA
19
Discussion
This study examined the ECG abnormalities and lipid profiles of
children with SCA. These children had higher levels of triglycerides
and lower levels of total cholesterol and LDL-C when compared
to suitable age- and gender-matched controls. In addition to
higher prevalence of LVH, they also had longer PR intervals, QRS
duration, heart rate and corrected QT interval, with the majority
(79%) having at least one identifiable ECG abnormality.
Although these findings are not entirely novel for adults
with SCA, the demonstration of a positive correlation between
triglyceride level and PR interval, as well as higher mean
triglyceride levels among SCA children with ECG abnormalities,
have not been reported in children. Our finding also supports
suggestions that (1) SCA children are at increased risk of
developing cardiac abnormalities and, (2) specific dyslipidaemic
syndrome, especially elevated levels of triglycerides, is a potential
biochemical marker of ECG abnormalities in SCA. As described
by Kato
et al.
,
19
progressive haemolysis-induced vasculopathy,
one of the two major subphenotypes associated with clinical and
laboratory manifestations of SCA, has been linked to endothelial
dysfunction and the subsequent development of reticulocytosis,
leg ulcers, priapism, stroke, elevated pulmonary arterial pressure
and cardiac abnormalities in sickle cell disease.
The prevalence of ECG abnormalities in children with SCA
in this study was 79%. This is comparable to some reported rates
among adult Nigerians with SCA.
20,21
Also, the finding of LVH
as the ECG abnormality seen in 71% of SCA children is similar
to many previous local reports.
20,21
It has also beeen documented
previously that Nigerian children with SCA have higher rates of
arrhythmias than their counterparts without SCA.
22
Abnormal
loading conditions associated with chronic anaemia lead to
chamber dilatation and myocardial remodelling, which progress
to ventricular dysfunction.
23
However, other factors such as
genetic variations or polymorphisms are also thought to be
involved in the dimensional and functional differences seen in
LV dysfunction in SCA.
23
The findings of T-wave abnormality consistent with lateral
ischaemia in children with SCA (12.9 vs 0%,
p
=
0.021) have
not been reported previously. This study also demonstrated
that PR interval was significantly prolonged, and mean QT
C
interval was significantly longer in patients with SCA than in the
controls. These are consistent with findings by Adebayo
et al.
,
Bode-Thomas
et al.
and Oguanobi
et al
.
1,2,21
The prolongation
of QT
C
interval, which implies abnormal repolarisation, can be
explained by the fact that patients with SCA experience recurrent
microscopic infarctions of the myocardium, especially with
repeated vaso-occlusion.
24
Bode-Thomas and co-workers have demonstrated that ECG
changes consistent with myocardial ischaemia are common in
children with SCA, especially during episodes of severe vaso-
occlusive crises, acute chest syndrome, and in those with elevated
pulmonary arterial pressure.
25,26
This may actually predispose
them to increased risk of cardiovascular mortality from
cardiac arrhythmias. Areas of micro-infarction are potential
arrhthmogenic sites with the possibility of generating malignant
arrhythmias such as ventricular and atrial tachyarrhthmias.
In this study, haematocrit levels had a negative correlation with
both QT and QT
C
intervals in children with SCA. Prolonged and
shortened QT
C
on ECG are both known risk factors for sudden
cardiac death.
27,28
Although, the exact mechanism of prolonged
QT
C
interval in sudden cardiac deaths in individuals with SCA
is largely unknown, it is speculated that chronic anaemia and
associated sub-acute cardiac ischaemia may be associated with
ventricular repolarisation defects, which ultimately prolong QT
C
intervals.
28
Specific dyslipidaemic subphenotype, especially elevated
triglyceride levels, in addition to having a positive correlation with
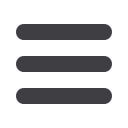
Table 4
.
Comparison of the sociodemographic and
baseline clinical characteristics of SCA children with
ECG abnormalities and those without abnormalities
Characteristics
Normal
ECG
pattern
Single
ECG
abnormality
Multiple
ECG
abnormalities p-value*
Number
13
19
30
Males,
n
(%)
9 (69.2)
11 (57.9)
19 (63.3)
0.806
Females,
n
(%)
4 (30.8)
8 (42.1)
11 (36.7)
Mean age
7.2
±
4.3 7.8
±
3.9 8.0
±
3.8 0.807
Age 2–5 years,
n
(%)
6 (46.2)
5 (26.3)
7 (23.3)
Age 6–10 years,
n
(%)
4 (30.8)
11 (57.9)
16 (53.3)
0.509
Age > 10 years,
n
(%)
3 (23.1)
3 (15.8)
7 (23.3)
Upper class,
n
(%)
2 (15.4)
9 (47.4)
7 (23.3)
Middle class,
n
(%)
5 (38.5)
6 (31.6)
8 (26.7)
0.165
Lower class,
n
(%)
6 (46.2)
4 (21.1)
15 (50.0)
≥ 3 pain/12 months,
n
(%)
6 (46.2)
9 (47.4)
14 (46.7)
0.998
ACS,
n
(%)
1 (7.7)
3 (15.8)
2 (6.7)
0.576
SBP (mmHg)
84.7
±
8.5 88.7
±
12.1 86.0
±
13.7 0.623
DBP (mmHg)
49.6
±
8.5 54.2
±
10.6 48.7
±
9.4 0.141
MAP (mmHg)
61.3
±
7.7 65.7
±
10.4 61.1
±
10.1 0.247
Pulse pressure (mmHg)
35.0
±
7.6 34.5
±
8.3 37.3
±
9.4 0.487
Weight (kg)
22.4
±
8.8 24.0
±
7.7 22.4
±
7.6 0.774
Height (m)
1.18
±
0.20 1.24
±
0.22 1.21
±
0.20 0.774
*
p-
values when the three groups were compared; SBP
=
systolic blood pres-
sure; DBP
=
diastolic blood pressure; MAP
=
mean arterial pressure; ACS
=
acute chest syndrome.
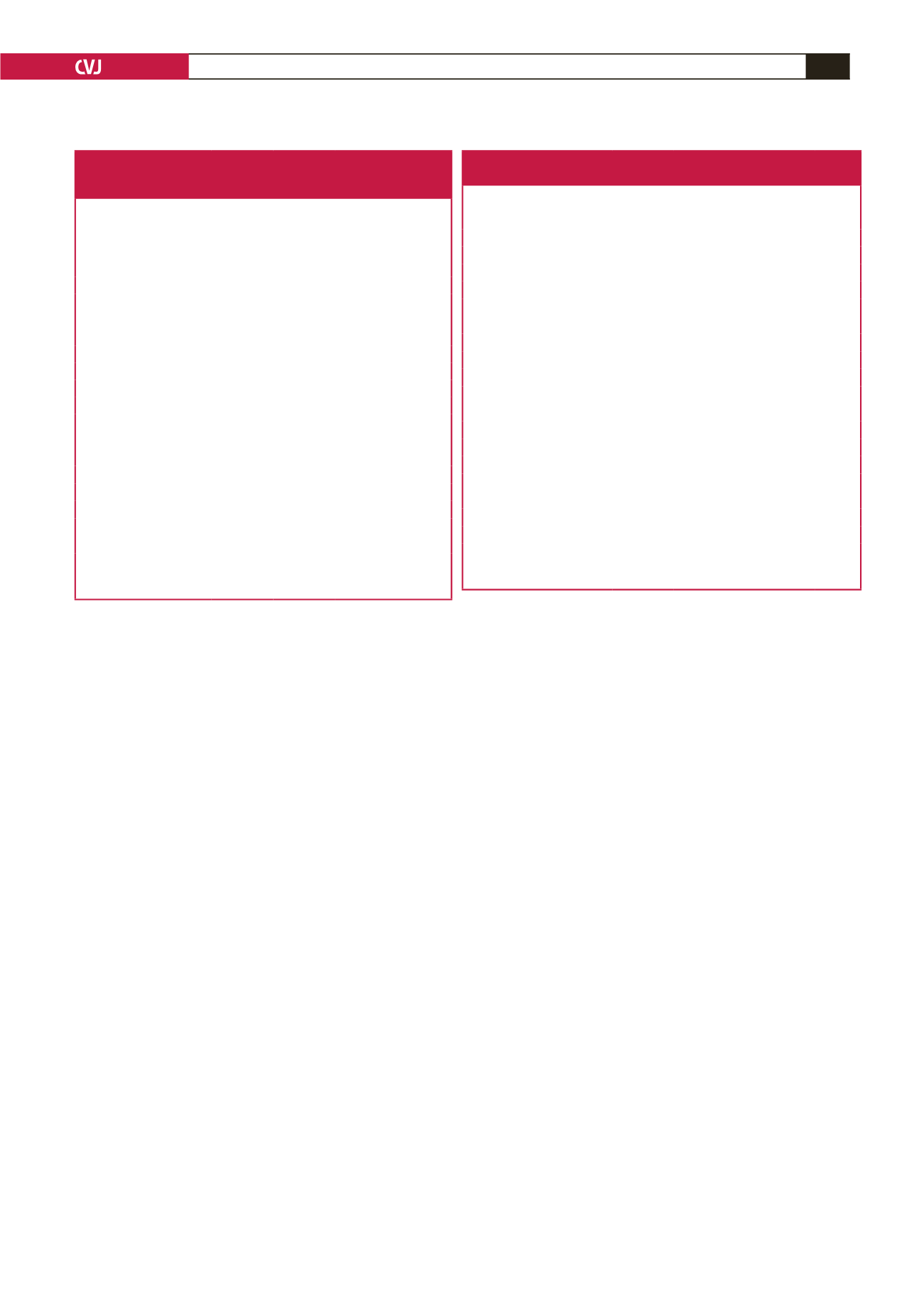
Table 5. Comparison of the baseline laboratory profiles of
SCA children with and without ECG abnormalities
Characteristics
Normal
ECG
pattern
Single
ECG abnor-
mality
Multiple ECG
abnormalities p-value*
Number
13
19
30
Haematocrit (%)
25.5
±
4.2 24.4
±
3.0 23.5
±
3.8 0.263
Leucocyte count (× 10
3
/mm
3
) 9.27
±
5.22 9.70
±
3.69 9.78
±
6.24 0.964
Platelet count (× 10
5
/ mm
3
)
2.24
±
0.89 2.33
±
1.09 2.02
±
0.39 0.710
Total bilirubin (µmol/l)
32.0
±
15.3 50.5
±
16.2 60.5
±
67.1 0.545
Direct bilirubin (µmol/l)
8.6
±
4.5 6.9
±
2.2 16.1
±
25.4 0.500
Indirect bilirubin (µmol/l)
23.4
±
11.7 43.6
±
14.7 44.4
±
42.7 0.421
Creatinine (mmol/l)
62.6
±
17.7 66.8
±
21.3 62.7
±
21.8 0.858
AST (IU/l)
20.3
±
17.3 23.8
±
17.2 22.9
±
14.6 0.938
ALT (IU/l)
5.0
±
4.8 10.9
±
7.1 17.3
±
9.2 0.045
Alkaline phosphatase
209.7
±
7.0 236.0
±
123.8 191.7
±
131.1 0.815
Total protein (g/dl)
66.8
±
8.0 69.8
±
10.6 73.4
±
8.7 0.472
Albumin (g/dl)
31.8
±
2.9 36.5
±
3.1 37.3
±
8.7 0.334
Total cholesterol (mmol/l)
2.62
±
0.49 2.52
±
0.30 2.64
±
0.46 0.639
HDL-C (mmol/l)
0.94
±
0.40 1.03
±
0.35 0.93
±
0.36 0.665
Triglyceride (mmol/l)
0.74
±
0.28 0.76
±
0.25 1.24
±
0.78 0.007
LDL-C (mmol/l)
1.33
±
0.41 1.24
±
0.69 1.27
±
0.63 0.914
Cholesterol:HDL-C ratio 3.40
±
1.74 2.78
±
1.44 3.18
±
1.31 0.461
*
p-
values by ANOVA to compare means of the three groups; ALT
=
alanine
transferase; AST
=
aspartate transferase; HDL-C
=
high-density lipoprotein
cholesterol; LDL-C
=
low-density lipoprotein cholesterol.

















