
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 5, September/October 2016
AFRICA
331
high incidence of severe hypertension owing to poor compliance
with medication and lifestyle-modification strategies. Often in
our setting, however, the patient may even be unaware of the
presence of hypertersion.
19
The exact mechanism for the higher
frequency of stroke in blacks remains unclear.
In our series, most patients presented during weekdays and
the majority during working hours. This pattern of presentation
may be attributed to the preference of patients or caregivers to
present at these times with the hope that they will receive better
care. Weekends and after hours are often characterised by the
constraints of understaffing and poor access to specialised
services.
10
This study revealed that the odds of dying were significantly
higher among those who presented during after-hours, compared
with those who presented during working hours. Therefore for
every 10 deaths among patients admitted during after-hours,
we would expect three among patients admitted during normal
working hours. Being hospitalised for more than 14 days was
also a predictor of mortality. However, being admitted over the
weekend was not found to be a predictor of mortality.
The significantly higher mortality rate registered during after-
hours may have been multifactorial. There are usually fewer
workers during after-hours and these tend to be juniors with less
clinical experience. Some of these may be filling in for regular
staff and may not have a good knowledge of the patients and the
internal workings of the particular unit. Handing-over sessions
may not be effectively implemented, resulting in serious gaps in
clinical knowledge that may adversely affect crucial management
decisions. Also, there tends to be fewer supervisors during
after-hours to provide oversight in various clinical scenarios.
20,21
Ancillary services such as laboratories and radiology, which
provide crucial support in the management of critically ill
patients, are usually less accessible during after-hours. These
factors may all have contributed to higher mortality rates being
recorded during after-hours.
Interestingly, the higher mortality rate was not recorded when
weekend admissions were compared with weekday admissions.
It has been noticed in our hospital that admission rates tend to
decline over the weekends. This may be due to the perception
within the populace that only skeletal services can be obtained
over the weekends. It is possible that the more critically ill
patients are taken to private hospitals during the weekend
instead of being brought to our centre. This might account for
the lack of difference between in-hospital mortality rates during
weekends compared with weekdays.
The higher mortality rates among those who were in hospital
for more than 14 days may have been linked to disease severity.
It is likely that those who remained in hospital for longer periods
suffered from more severe forms of disease that led inexorably
to poorer outcomes. This finding is in agreement with a report
that highlighted a strong correlation between the high Acute
Physiology and Chronic Health Evaluation (APACHE) III and
multiple-organ dysfunction syndrome scores and prolonged
length of stay for critically ill patients in the intensive care
unit.
22,23
Our findings suggest that healthcare providers in Nigeria
should consider the potential increase in mortality rate that may
arise as a consequence of uneven staffing patterns, especially
during after-hours. The economic implications of striving to
achieve and maintain a consistent level of staffing naturally come
to the fore. Although it has been suggested that maintaining high
levels of staffing may sometimes be economical, it is often not
feasible. However, innovation is required to ensure that such
re-organisation represents an efficient use of scarce resources.
A limitation of this study is that owing to the high cost and
sometimes unavailability of facilities for neuro-imaging, the
majority of patients with stroke did not have imaging records,
so the different types of stroke could not be clearly determined.
Conclusion
Our findings confirm that outcome is poor for cardiovascular
admissions during after-hours but not during weekends. It is
suggested that patients may deliberately be avoiding seeking
medical care in public institutions during weekends. The increase
in CVD mortality may be as a consequence of uneven staffing
patterns, especially during after-hours. Healthcare providers in
Nigeria should strive to achieve and maintain a consistent level
of staffing, especially during after-hours and weekends, despite
the economic implications. This is often not feasible, therefore
innovation is required to ensure that such re-organisation
represents an efficient use of scarce resources.
References
1.
Bell CM, Redelmeier DA. Mortality among patients admitted to hospi-
tals on weekends as compared to weekdays.
N
Engl
J Med
2001;
345
:
663–668.
2.
Freemantle N, Richardson M, Wood J,
et
al.
Weekend hospitalization
and additional risk of death: an analysis of in-patient data
J R Soc Med
2012;
105
: 74–84.
3.
DeCoster C, Roos NP, Carriere KC, Peterson S. Inappropriate hospital
use by patients receiving care for medical conditions: targeting utiliza-
tion review.
Can Med Assoc
J 1997;
157
: 889–896.
4.
Marco J, Barba R, Plaza S,
et al
. Analysis of mortality of patient admit-
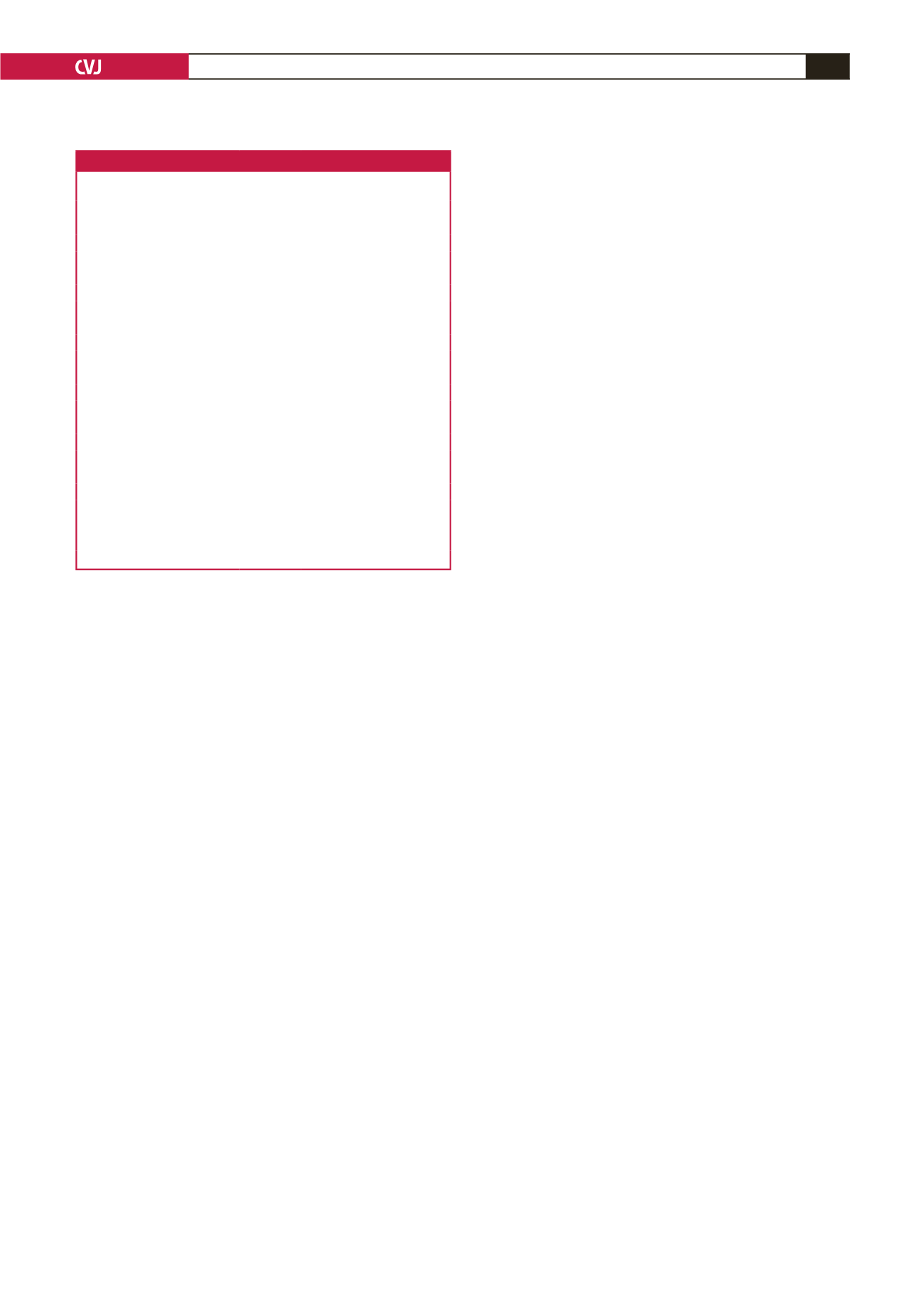
Table 4. Predictors of poor outcome among all patients
Variable
Odds ratio
95% confidence
interval
p
-value
Age (years)
≤
55
1.89
0.73–4.86
0.19
>
55
1
Gender
Female
1.05
0.44–2.47
0.92
Male
1
Route of admission
ED
1.01
0.31–3.34
0.99
MOPD
1
Presentation time
After hours
3.37
0.31–0.56
0.04*
Working hours
1
Day presented
Weekday
1.10
0.38–3.21
0.86
Weekend
1
Causes of heart failure
Other
0.83
0.33–2.05
0.68
Hypertension
1
Duration of admission (days)
≤
14
0.22
0.08–0.59
0.003*
>
14
1
ED: emergency department, MOPD: medical out-patients’ department.

















