
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 5, September/October 2016
e2
AFRICA
tachycardia with no ischaemic changes. The hs-troponin T level
was 0.154 ng/ml and pro-BNP concentration was also elevated to
22 842 ng/l. However, 72 hours later he showed no improvement
in his left ventricular function and despite increasing doses of
inotropic support, he remained hypotensive.
A decision was therefore made to insert the Tandem Heart left
ventricular assist device (LVAD). The patient’s haemodynamics
were stabilised with the LVAD and the inotropes were gently
weaned. Therapy was commenced with carvedilol, enalapril and
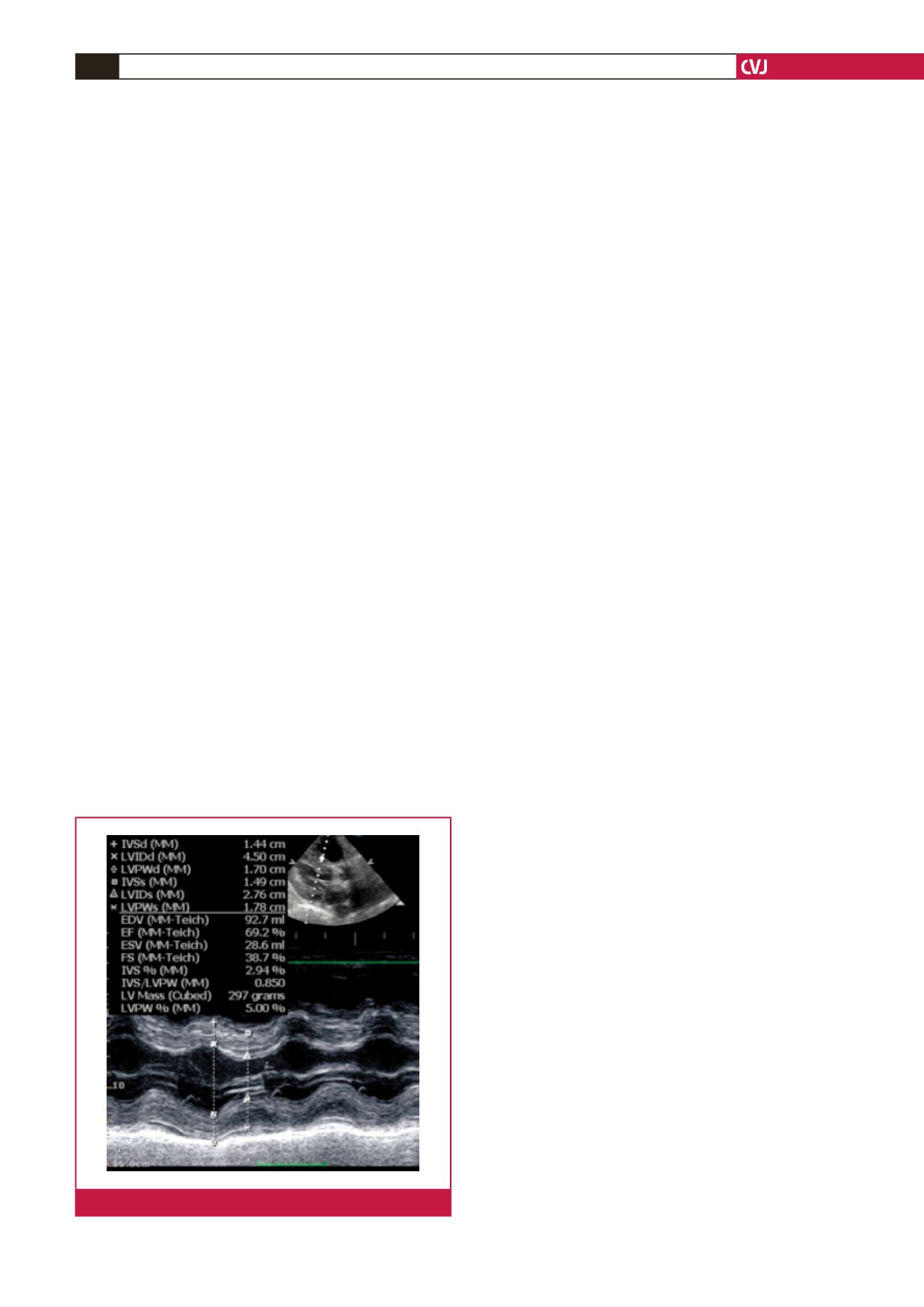
spironolactone. His left ventricular function gradually improved
(Fig. 2) and he was weaned from the LVAD after nine days.
He recovered well and at discharge 25 days post
transplantation, his LVEF was 69%. At the four-month post-
transplantation review he remained asymptomatic and his LVEF
had improved to 75%.
Discussion
Takotsubo cardiomyopathy or acute non-ischaemic stress
cardiomyopathy is a well described cause of transient acute left
ventricular dysfunction, leading to haemodynamic instability
and ventricular arrhythmias. At our transplantation centre with
an experience of over 240 liver transplants, this is the first case
of acute stress cardiomyopathy that we have encountered post
liver transplantation.
Patients with cirrhosis requiring liver transplantation
demonstrate an impaired systolic and diastolic response to stress,
as well as electrophysiological abnormalities, a condition termed
cirrhotic cardiomyopathy.
1
These cardiac disturbances are most
likely mediated by decreased beta-adrenergic receptor density
and dysfunction, increased circulating inflammatory mediators
with cardiodepressant properties and repolarisation changes.
1
Liver transplant patients are therefore more vulnerable to peri-
operative cardiac stress.
The prevalence of Takotsubo cardiomyopathy post liver
transplantation has been reported to range between one and
7%. In a large retrospective review of 1 460 liver transplant
records in a single centre, the overall prevalence of Takotsubo
cardiomyopathy was found to be 1.2%.
2
Furthermore they
found an association of Takotsubo cardiomyopathy with higher
MELD scores, renal insufficiency and malnutrition prior to
transplantation. Also 52% of these patients had a significant
history of alcohol abuse.
2
The cause of the acute left ventricular decompensation post
transplantation in our patient is not clear. The patient’s coronary
angiogram was normal prior to transplantation. It is possible
that the underlying propensity to an impaired ventricular
response to stress, history of alcohol abuse as well as the acute
increase in left ventricular afterload secondary to aortic cross
clamping during surgery may have contributed to the acute
global left ventricular dysfunction.
Strategies for managing acute left ventricular dysfunction
post liver transplantation are not well defined. Standard
approaches with diuretics, and inotropic and vasopressor
support are the mainstays of initial management. However, if
these fail, percutaneous devices for circulatory support need to
be considered.
Intra-aortic balloon pumps are used acutely in the setting
of hypotensive crises secondary to acute coronary syndromes.
However, they are rarely considered as a bridge to myocardial
recovery.
LVAD implantation is a well-described therapy in highly
selected patients with refractory end-stage heart failure.
3
They
are also used as a bridge to myocardial recovery following acute
myocardial injury where recovery of myocardial function is
expected.
We postulated that our patient may have suffered a
non-ischaemicstresscardiomyopathy.Takotsubocardiomyopathy
occurs predominantly in females and the interesting aspects
of this case are that it occurred in a male patient, as well as
occurring post liver transplantation. The patient showed a poor
response to inotropic and vasopressor support and therefore the
decision for LVAD implantation was made early, which possibly
contributed to his rapid recovery.
Conclusion
Thus far there is only one reported case of the successful use of
ventricular assist device for acute left ventricular decompensation
post liver transplantation.
4
Our case study demonstrates
the importance of thorough pre-operative assessment of
transplantation patients and the multi-disciplinary support
necessary for those patients who deteriorate in the immediate
post-transplant period.
We acknowledge the following colleagues, who were also involved in the
management of the patient: N Patel, M Chohan, P Williams, Z Adham and
R Britz.
References
1.
Raval Z, Harinstein ME, Skaro AI, Erdogan A, DeWolf AM, Shah SJ,
et al
. Cardiovascular risk assessment of the liver transplant candidate.
J
Am Coll Cardiol
2011;
58
(3): 223–231.
2.
Yataco ML, Difato T, Bargehr J, Rosser BG, Patel T, Trejo-Gutierrez
JF,
et al
. Reversible non-ischaemic cardiomyopathy and left ventricular
Fig. 2.
Left ventricular recovery post LVAD implantation.

















