
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 2, March/April 2017
AFRICA
109
used as grafts. An aortic arterial and unicaval two-stage venous
cannulation was performed on patients in the on-pump CABG
group; an antegrade cardioplegia cannula and a venting cannula
were placed into the aortic root, and a retrograde cardioplegia
cannula was placed into the coronary sinus via the right atrium.
Myocardial contraction was stopped in the diastolic phase
using isothermic hyperkalaemic blood cardioplegia via an
antegrade cannula, and myocardial protection was achieved
using isothermic hyperkalaemic blood cardioplegia via a
retrograde cannula, with the effect of systemic hypothermia.
Haemodynamic monitoring was continued in the intensive care
unit (ICU) and the patients underwent haemodialysis. Patients
with early mortality (group 1) were compared with surviving
patients (group 2) for peri-operative parameters (Table 1).
Statistical analysis
The Statistical Package for Social Sciences (SPSS) for Windows
15.0 was used to evaluate the findings of the study, and the
Kolmogorov–Smirnov test was used to evaluate the coherence
of the normal distribution of the study parameters. Descriptive
statistical methods (standard deviation, frequency and mean)
were used.
The quantitative parameters were evaluated in two parts. The
Student’s
t
-test was used for normally distributed parameters,
and the Mann–Whitney
U
-test was performed for non-normally
distributed parameters. The Wilcoxon test was used to compare
the parameters in both groups.
The chi-squared, Fisher’s exact and McNemar’s tests were
used to compare qualitative parameters;
p
<
0.05 was accepted
as significant. Univariate and multivariate analysis were used to
determine independent risk factors.
Results
Pre-operative findings were analysed according to demographic
characteristics. The mean age of the patients who died was
statistically significantly higher in the pre-operative evaluation (
p
<
0.05), as were the mean age and EuroSCORE (
p
<
0.05). The
New York Heart Association (NYHA) functional capacity of
the patients was found to be highly significantly correlated with
mortality rate of patients (
p
<
0.01). Significantly more of the
patients who died were in NYHA class III–IV (OR: 3.333; 95%
CI: 1.199–9.268).
There was a statistically significant difference with regard to
mortality rate between the types of surgery (
p
<
0.05). Significantly
more patients who received emergency surgery died (OR: 10.333;
95% CI: 1.012–105.487). There was also a statistically significant
difference in the incidence of hypertension (
p
<
0.05) between
the patients who died and those who survived. The incidence of
hypertension in patients who died was significantly higher than
in those who survived (Table 2).
The ICU length of stay and extubation time of patients who
died were statistically significantly longer than those of surviving
patients (
p
<
0.01).The incidence of pneumonia in patients who
died was statistically significantly higher than in those who
survived (
p
<
0.01; Table 3).There was also a significant difference
in pre- and postoperative values of creatinine kinase-MB (CK-MB)
and troponin between living and dying patients (Table 4).
The myocardial infarction (MI) rate in the pre-operative
period was statistically significantly higher in patients who
died than in surviving patients (
p
<
0.05; OR: 3.400; 95% CI:
1.027–11.257). The MI rate in the postoperative period was also
statistically significantly higher in deceased cases than in the
surviving patients (
p
<
0.01; OR: 8.800; 95% CI: 2.753–28.134).
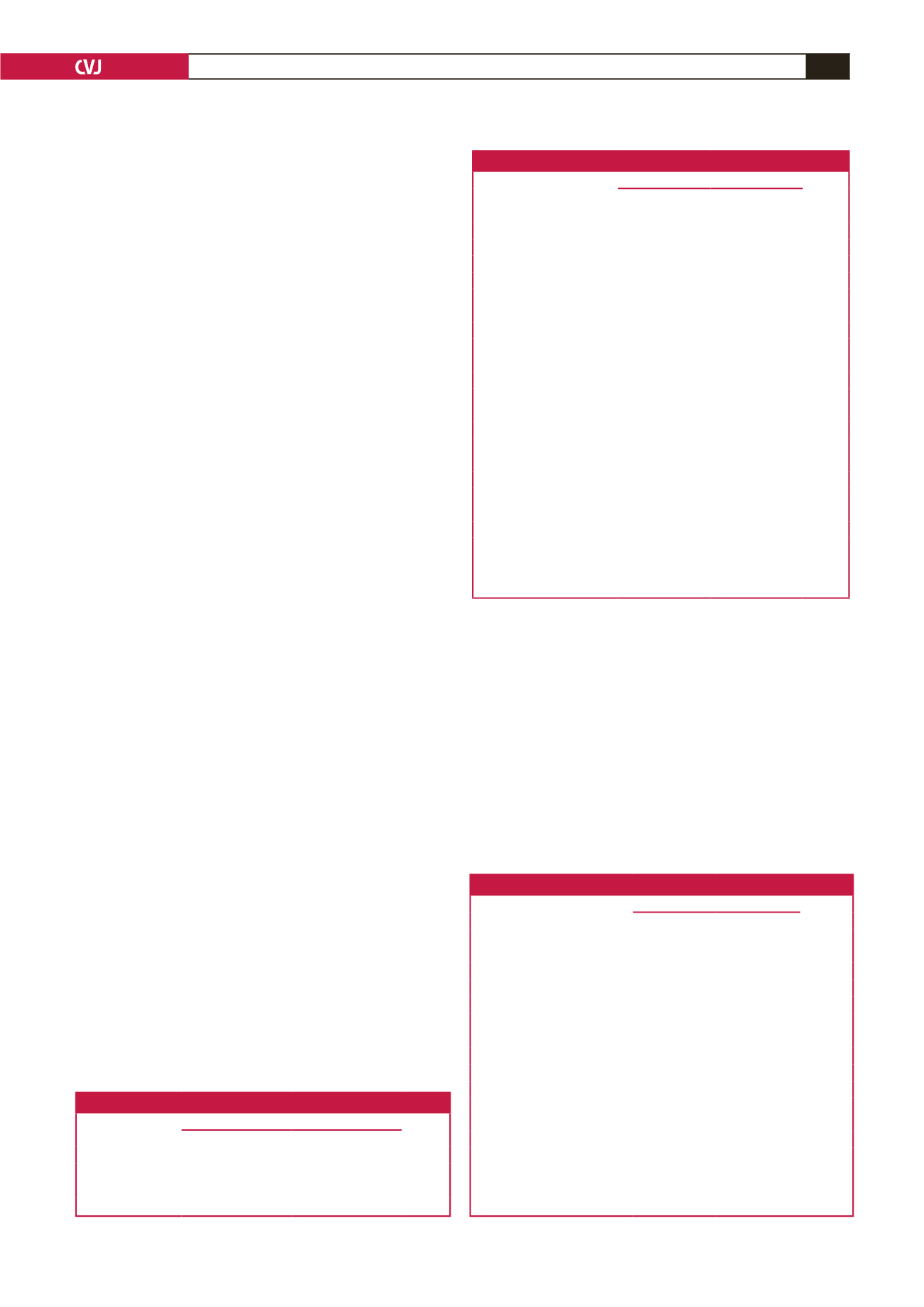
Table 1. Evaluation of mortality by demographic characteristics
Mortality
p
-value
Yes, Mean
±
SD No, Mean
±
SD
Age
63.47
±
9.89
58.17
±
9.66
0.033*
Female,
n
(%)
7 (33.3)
17 (27.0)
0.577
Male,
n
(%)
14 (66.7)
46 (73.0)
Student’s
t
-test for age; chi-squared test for gender; *
p
<
0.05.
Table 2. Assessments for pre-operative mortality
Mortality
p
-value
Yes, Mean
±
SD No, Mean
±
SD
EuroSCORE
9.28
±
3.39 (9)
7.52
±
2.58 (8)
0.040*
Ejection fraction (%)
48.33
±
12.28 (50) 53.33
±
10.85 (55) 0.103
NYHA class,
n
(%)
1
0 (0.0)
16 (25.4)
0.004**
2
9 (42.9)
29 (46.0)
3
10 (47.6)
18 (28.6)
4
2 (9.5)
0 (0.0)
Canada class,
n
(%)
1
0 (0.0)
1 (1.6)
0.751
2
11 (52.4)
30 (47.6)
3
9 (42.9)
31 (49.2)
4
1 (4.8)
1 (1.6)
Surgery,
n
(%)
Elective
18 (85.7)
63 (100.0)
0.014*
Emergency
3 (14.3)
0 (0.0)
Smoker,
n
(%)
7 (33.3)
34 (54.0)
0.101
Diabetes,
n
(%)
11 (52.4)
37 (58.7)
0.611
Hypercholesterolaemia,
n
(%)
6 (28.6)
19 (30.2)
0.890
Hypertension,
n
(%)
13 (61.9)
54 (85.7)
0.019*
PAD,
n
(%)
3 (14.3)
16 (25.4)
0.292
COPD,
n
(%)
7 (33.3)
18 (28.6)
0.679
Mann-Whitney
U
-test for euroSCORE and ejection fraction; chi-squared test
for the other variables.
PAD: peripheral arterial disease, COPD: chronic obstructive pulmonary disease.
Table 3. Assessments for intra-operative mortality
Mortality
p
-value
Yes, Mean
±
SD No, Mean
±
SD
Transfusion (units)
2.30
±
1.62
1.79
±
1.24
+
0.160
Extubation time (min)
66.90
±
110.99 15.03
±
8.87
+
0.001**
ACC (min)
77.00
±
35.37 61.24
±
22.23
+
0.166
TPT (min)
119.17
±
45.30 99.90
±
26.38
+
0.183
Hypothermia (°C)
30.87
±
2.19
30.98
±
1.72
+
0.861
Chest tube drainage (ml)
911.90
±
580.06 652.38
±
386.61
+
0.067
ICU stay (day)
11.57
±
9.08
3.93
±
2.92
+
0.001**
Postoperative creatinine (mg/dl)
4.56
±
2.26
5.48
±
2.13
+
0.097
(μmol/l)
(403.10
±
199.78) (484.43
±
188.29)
Redo surgery,
n
(%)
1 (4.8)
1 (1.6)
++
0.440
Postoperative dialysis
19 (90.5)
57 (90.5)
++
1.000
Complete revascularisation,
n
(%)
12 (57.1)
41 (65.1)
++
0.514
Pneumonia,
n
(%)
10 (47.6)
2 (3.2)
++
0.001**
ACC: aortic cross clamp time, TPT: total perfusion time; ACC, TPT and hypo-
thermia related to on-pump group (54 patients).
+
Student’s
t
-test for chest tube drainage and postoperative creatinine levels;
Mann–Whitney
U
-test for other variables;
++
Chi-squared test and/or Fisher’s exact
test; **
p
<
0.01.

















