
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 2, March/April 2017
114
AFRICA
than in women (6.7%). All patients were symptomatic, and the
majority (77.5%) presented with dyspnoea (NYHA functional
class III or IV), peripheral oedema, orthopnoea, palpitations
and basal crepitations. Overall, the median (IQR) systolic
and diastolic blood pressures were 120.0 (103.8–133.5) and 74
(67–81.5) mmHg, respectively. Because of cost limitations, the
NT-proBNP level was determined in only 107 patients, with a
median value (IQR) of 3 314 (1 360–6 506) pg/ml.
More than one-half (54.9%) of the patients were hypertensive.
Hypertension was more commonly reported in the women than
the men (64.0 vs 47.1%,
p
<
0.05). A prior diagnosis of diabetes
mellitus was present in 30 (15.5%) patients and often coexisted
with hypertension. Moderate to severe renal dysfunction was
detected in 60 (31.1%) patients. Forty-five (23.3%) patients had
a haemoglobin level
<
10 g/dl, a finding that was commonly
seen among those with chronic kidney disease. Overall, anaemia
was more common in the women than men. HIV results were
available for 180 (93.3%), and about a third (33.9%) of these
patients were HIV positive.
The mean LVEF was 41.7%, and about two-thirds (64.8%) of
the patients had HF with significant systolic dysfunction (LVEF
<
45%). Seventy-three (37.8%) patients presented with severely
depressed LV function (LVEF
<
30%), which was more common
in men than women (44.2 vs 30.3%,
p
<
0.05). Left atrial diameter
was enlarged to a mean value of 43 mm, and moderate to severe
mitral and tricuspid regurgitation was common (31.6 and 40.4%,
respectively). Other less common valvular disorders found
were mitral stenosis, aortic regurgitation and aortic stenosis.
The commonest causes of HF were hypertensive heart disease
(40.4%), dilated cardiomyopathy (19.6%), cor pulmonale (9.8%),
valvular heart disease (9.3%) and pericardial disease (6.2%).
Overall, right ventricular dysfunction was common, present
in 86 (44.6%) patients, and often coexisted with left ventricular
systolic dysfunction. Pericardial disease, dilated cardiomyopathy
and right HF were more common in men while hypertensive
and valvular HF were more common in women. Although
peripartum cardiomyopathy only accounted for 4.1% of all
cases of HF, it turned out to be the third commonest cause
of HF among female patients, occurring in eight (9%) of all
female patients. The mean age of patients with peripartum
cardiomyopathy was significantly lower than the other female
patients (32
±
7.3 vs 57
±
16.8 years,
p
<
0.01). Patients with
pericardial disease were more likely to be HIV positive than
those with other types of HF. Ischaemic heart disease was found
in 5.7% of the patients and was more common in women and
patients with hypertension and diabetes. Other causes of HF in
the cohort included amyloidosis, hypertrophic cardiomyopathy,
thyroid heart disease and congenital heart disease.
Table 2 shows patient outcomes in the wards, discharge
medications, and outcomes over the six months of post-
discharge follow up. Overall, diuretics, beta-blockers, angiotensin
converting enzyme (ACE) inhibitors or angiotensin receptor
blockers, and spironolactone were often prescribed to patients at
discharge. The most commonly used medications were carvedilol,
bisprolol, enalapril, telmisartan and furosemide.
In-hospital mortality rate of HF patients was 10.9%, and was
associated with hyponatraemia (
p
= 0.023), elevated NT-proBNP
(
p
= 0.001) and urea levels (
p =
0.013), and hyperuricaemia (
p
=
0.036). The median length of stay was nine days (IQR 5–15). The
LOS was similar regardless of the NYHA functional status of HF
after hospital discharge. After 30 days, three (1.6%) patients could
not be traced telephonically and were declared lost to follow up.
Seven patients (4.1%) died within 30 days of discharge from
hospital. Overall, 28/190 (14.7%) patients died within 30 days of
admission. By the 90th day after admission, 10 (5.2%) patients
were lost to follow up, and of the rest, 47/183 (25.7%) were
deceased. A total of 11 (5.7%) were lost to follow up by six
months of admission, and the 180-day case fatalities from HF
were 30.8%. Mortality at 180 days was significantly associated
with increasing age, lower haemoglobin level, lower eGFR,
hyponatraemia, higher NT-proBNP levels, and prolonged
hospital stay (Table 3).
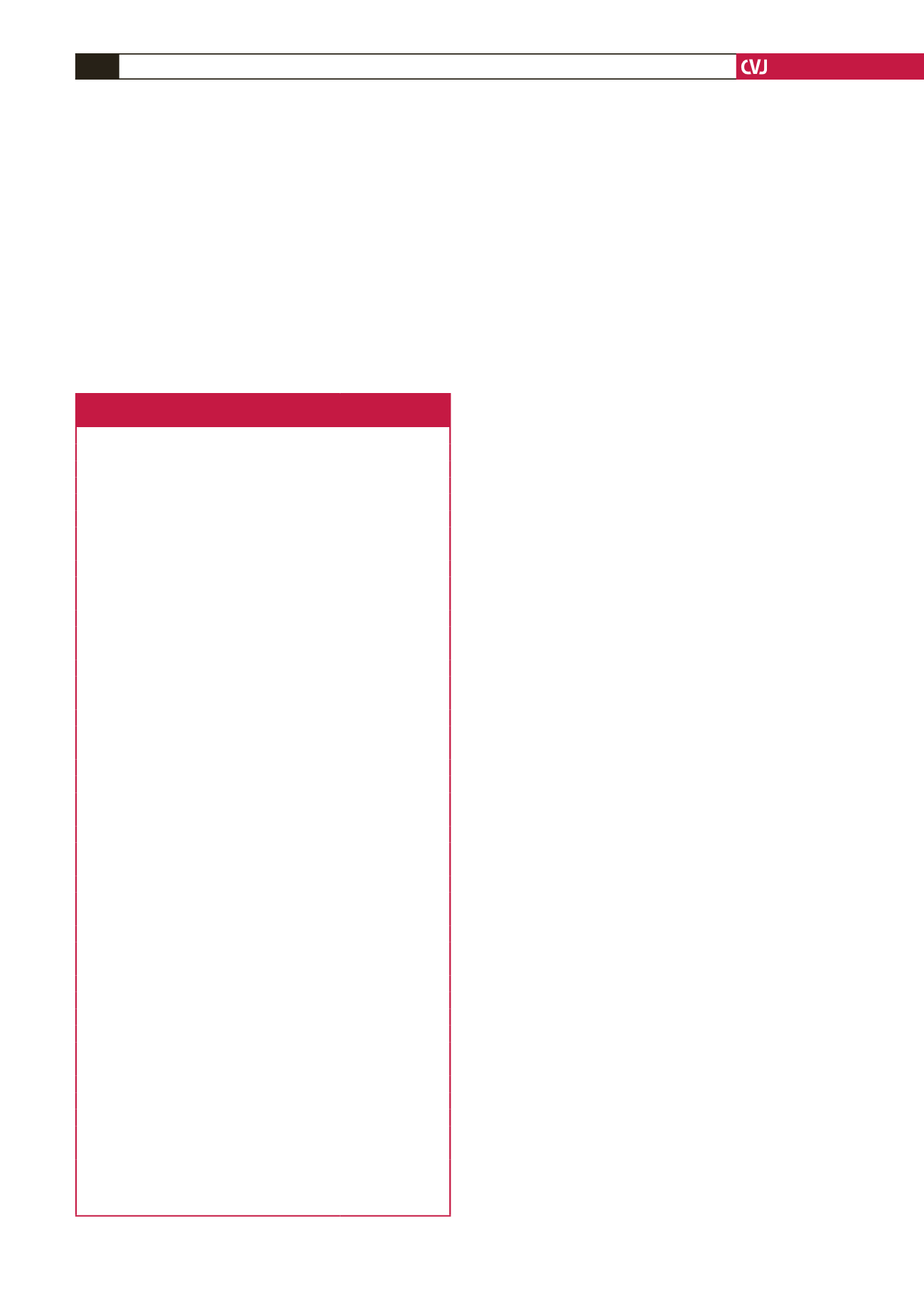
Table 1. Clinical and demographic characteristics
of patients admitted with heart failure
Characteristics
n
= 193
Mean age (years) (SD)
54.2
±
17.1
Male gender,
n
(%)
104 (53.9)
Medical history,
n
(%)
Hypertension
106 (54.9)
Prior type 2 diabetes
30 (15.5)
Renal failure
28 (15.0)
Rheumatic heart disease
21 (10.9)
Ischaemic heart disease
11 (5.7)
Stroke
19 (9.8)
Atrial fibrillation
19 (9.8)
HIV positive
61 (33.9)
Symptoms,
n
(%)
Shortness of breath
178 (92.2)
NYHA II
40 (22.5)
NYHA III
94 (52.8)
NYHA IV
44 (24.7)
Orthopnoea
151 (78.2)
Peripheral oedema
148 (76.7)
Paroxysmal nocturnal dyspnoea
152 (78.8)
Physical findings
Mean heart rate (bpm) (SD)
95.1
±
21.2
Median systolic blood pressure (mmHg) (Q1–Q3)
120.0 (103.8–133.5)
Median diastolic blood pressure (mmHg) (Q1–Q3)
74 (67–81.5)
Murmur,
n
(%)
76 (39.4)
Cyanosis,
n
(%)
7 (3.6)
Pedal oedema,
n
(%)
132 (68.4)
Elevated jugular venous pressure,
n
(%)
127 (65.8)
S3 gallop,
n
(%)
72 (37.3)
Basal crepitation,
n
(%)
126 (65.3)
Hepatomegaly,
n
(%)
100 (52.6)
Ascites,
n
(%)
43 (23.8)
Pleural effusion,
n
(%)
31 (16.1)
Laboratory tests
Mean haemoglobin (g/dl) (SD)
12.0
±
2.96
Creatinine (µmol/l) median (Q1–Q3)
98.0 (70–137.5)
Urea (mmol/l) median (Q1–Q3)
8.3 (4.9–13.7)
Mean sodium (mmol/l) (SD)
134.1
±
6.8
Mean potassium (mmol/l) (SD)
4.4
±
0.9
eGFR (ml/min/1.73 m
2
) median (Q1–Q3)
75.9 (52.5–112.4)
Echocardiography
Mean LVEF (%) (SD)
41.8
±
20.0
Mean LA (mm) (SD)
43
±
9
Mean IVSD (mm) (SD)
12.9
±
4.1
LVEF, left ventricular ejection fraction; eGFR, glomerular filtration rate; IQR,
interquartile range; SD, standard deviation; Q, quartile; NYHA, New York
Heart Association functional class; LVEF, left ventricular ejection fraction, LA,
left atrium; IVSD, interventricular septum diameter.

















